JACC:修复心脏瓣膜 开创性H-MVRS安全有效
2017-11-02 常路 环球医学
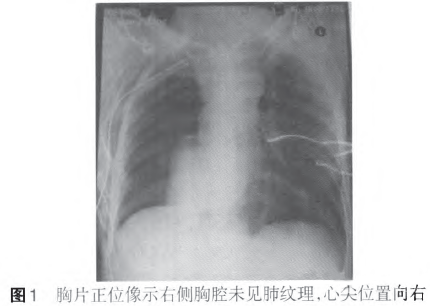
一项新研究发现,修复心脏瓣膜的开创性医疗设备安全有效,能降低常规二尖瓣手术的侵袭性和副作用。美国马里兰大学医学院(UMSOM)开发的基于技术的图像引导装置即Harpoon二尖瓣修复系统(H-MVRS)通过肋骨之间的小开口进行部署,并在维持心脏的同时进行修复。相关报告发表在《JACC》。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












还是缘对缘的夹合术,双孔。并不新鲜。
46
#JACC#
27
#心脏瓣膜#
29
#ACC#
23
#瓣膜#
22
学习了谢谢作者分享!
53