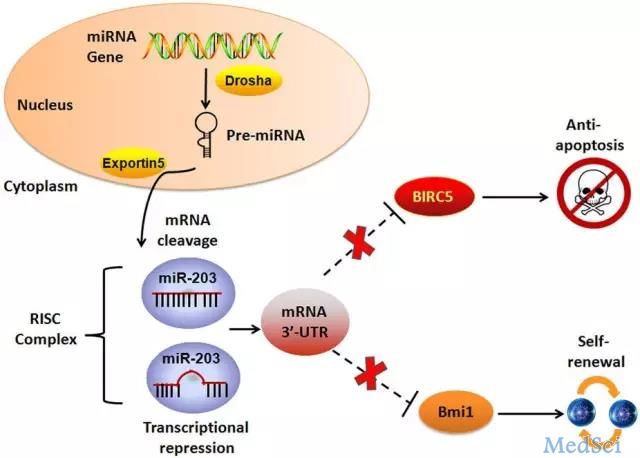
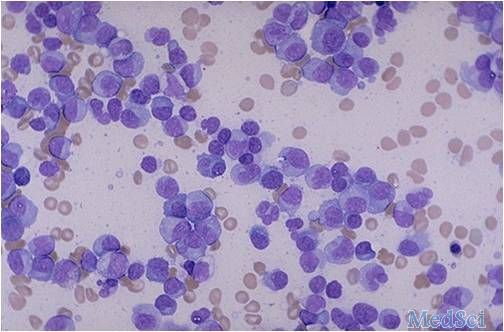
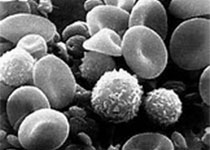
Sci Rep:miR-203通过靶向生存素与Bmi-1抑制白血病干细胞的增殖与自我更新
2017-08-07 佚名 Nature自然科研
《科学报告》发表一篇名为miR-203 inhibits proliferation and self-renewal of leukemia stem cells by targeting survivin and Bmi-1的文章,对急性骨髓性白血病治疗过程中的耐药性做出了机理解释。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#白血病干细胞#
64
#miR#
0
#自我更新#
41
好文章.好思路.
46
学习了
51
非常好的文章,学习了,很受益
58
谢谢分享,学习了
54
学习了新知识
58
学习,谢谢分享
26
文章真好,赞赞赞
30