Stroke:动脉瘤性蛛网膜下腔出血的最佳脑灌注压和脑组织氧含量
2022-11-02 MedSci原创 MedSci原创
动脉瘤蛛网膜下腔出血患者在DCI前的时期,PbtO2与患者CPP与CPPopt的偏差之间存在非线性关系
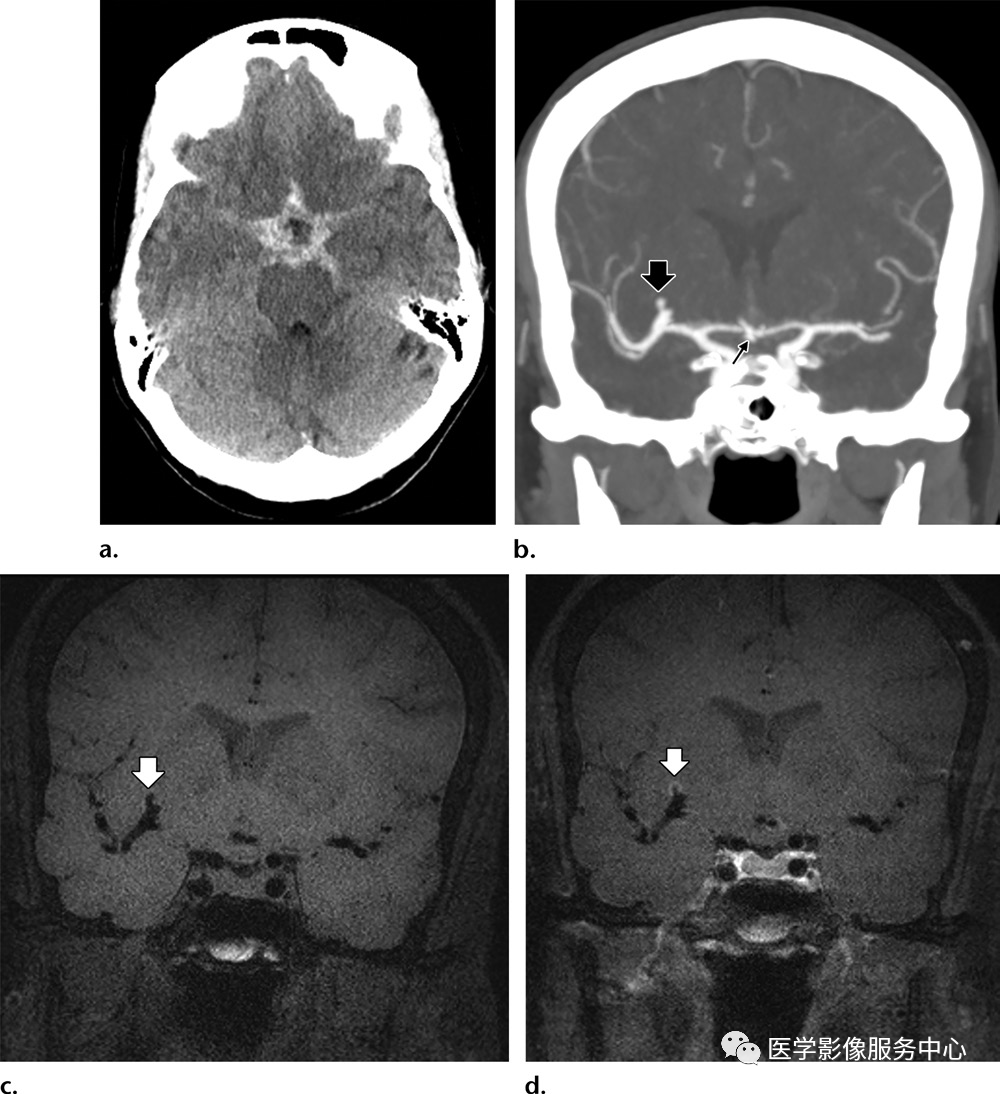
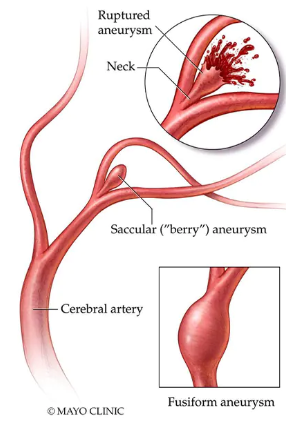
为防止急性神经损伤后的二次损伤,以脑自主调节的最佳脑灌注压为目标(CPPopt)已越来越受到重视。脑组织氧合度(PbtO2)可以识别脑血流不足和继发性脑损伤。界定动脉瘤性蛛网膜下腔出血后CPPopt和PbtO2之间的关系可能会导致(1)从机理上了解基于CPPopt的策略是否和如何有益,(2)建立对PbtO2作为充分或最佳局部灌注的辅助监测的支持。
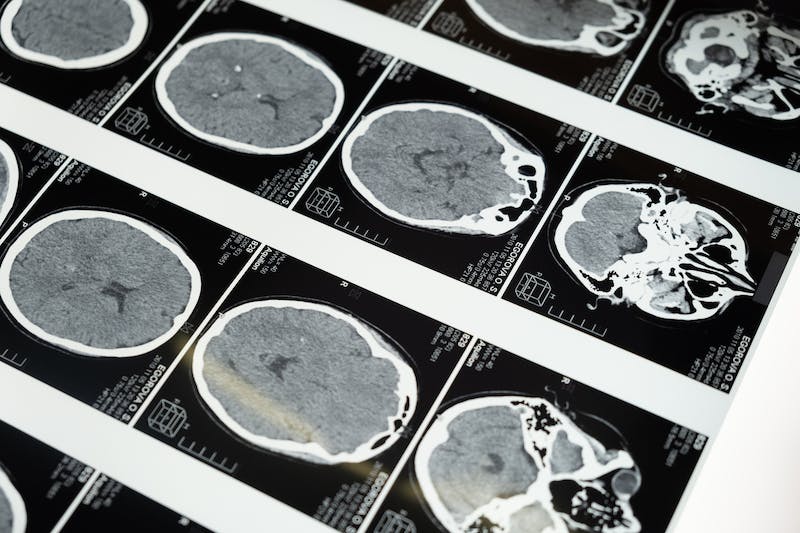
有学者对前瞻性收集的2个中心的动脉瘤性蛛网膜下腔出血患者的数据集进行了回顾性分析,无论后来是否诊断为迟发性脑缺血(DCI)。CPPopt被计算为与最低压力反应性指数(平均动脉压和颅内压的移动相关系数)相对应的脑灌注压(CPP)值。使用自然曲线回归分析研究了(每小时)deltaCPP(CPP-CPPopt)和PbtO2的关系。脑组织缺氧被定义为PbtO2<20 mmHg。

结果共有131名患者被纳入,中位数为44.0(四分位数范围,20.8-78.3)小时的CPPopt/PbtO2数据点。回归图显示PbtO2和deltaCPP之间存在非线性关系(P<0.001),deltaCPP<0mmHg时PbtO2下降,deltaCPP≥0mmHg时PbtO2稳定,不过个体差异很大。脑组织缺氧(占所有测量值的34.6%)在deltaCPP<0 mmHg时更为频繁。这些动态变化在有或没有DCI的患者中是相似的。
综上,动脉瘤蛛网膜下腔出血患者在DCI前的时期,PbtO2与患者CPP与CPPopt的偏差之间存在非线性关系。CPP值低于计算的CPPopt与较低的PbtO2有关。尽管如此,PbtO2测量的性质很复杂,而且变异性很大。
参考文献:
Optimal Cerebral Perfusion Pressure and Brain Tissue Oxygen in Aneurysmal Subarachnoid Hemorrhage. https://doi.org/10.1161/STROKEAHA.122.040339Stroke. 2022;0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














感谢分享#期刊论坛#
50
转发学习
43
感谢分享
39
学习受益
47
认真学习~~
38