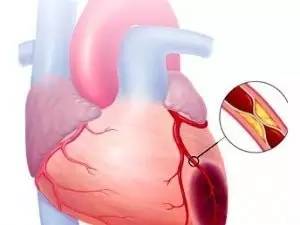
冠心病合并颈动脉狭窄专家共识的十大要点:四分之一冠心病患者颈动脉狭窄>50%
2016-12-26 卢芳 中国循环杂志
冠心病与颈动脉狭窄共患率不低,在冠脉病变患者中颈动脉狭窄>50%的发生率达25.4%;在颈动脉狭窄患者中冠心病患病率为13%~86%。为了能够促进临床实践更好地处理这两种疾病并存情况,中国医疗保健国际交流促进会血管疾病高血压分会专家共识组近期发布了《冠心病合并颈动脉狭窄的处理策略专家共识》。以下为其中要点: 1. 已确诊冠心病患者,行颈动脉听诊和颈动脉超声检查,如为明确阳性,需
冠心病与颈动脉狭窄共患率不低,在冠脉病变患者中颈动脉狭窄>50%的发生率达25.4%;在颈动脉狭窄患者中冠心病患病率为13%~86%。为了能够促进临床实践更好地处理这两种疾病并存情况,中国医疗保健国际交流促进会血管疾病高血压分会专家共识组近期发布了《冠心病合并颈动脉狭窄的处理策略专家共识》。
以下为其中要点:
1. 已确诊冠心病患者,行颈动脉听诊和颈动脉超声检查,如为明确阳性,需进一步行无创影像学检查,必要时行颈动脉造影。
2.已确诊颈动脉狭窄患者,问诊冠心病病史,并行心电图检查;可疑者如无禁忌建议行运动负荷心电图和(或)冠脉CT检查,如有明确的阳性发现,行冠状动脉造影检查。
3. 对于冠心病与颈动脉狭窄并存者,若病情平稳,药物治疗下无症状发作或偶有轻度症状发作,如狭窄病变程度不重,可以临床随访观察并强化药物治疗,3~6 个月复查1 次。
4. 对于有明显症状的患者,如以冠心病症状为主,应先行冠脉血管重建;以颈动脉症状为主,应先行颈动脉血管重建治疗。二者均不稳定,可考虑同期血管重建。
5. 对适合PCI和颈动脉支架指征者,一般先行PCI,病情稳定后择期行颈动脉支架,时间间隔3天以上为宜,如PCI 后有并发症,要待到并发症稳定或治愈后方可考虑颈动脉支架;如果病情允许或者病情需要,如病变简单,技术可靠,同期介入并非禁忌。
6. 若患者需冠脉搭桥,也需治疗颈动脉狭窄,一般情况下优先选择提前或同期植入颈动脉支架/行颈动脉内膜剥脱术和冠脉搭桥;但提前行颈动脉剥脱术和冠脉搭桥,只适合于冠状动脉病变稳定的患者。
7. 抗凝抗血小板策略:
(1)PCI+颈动脉支架:抗栓治疗策略参照单纯PCI的抗栓治疗。
(2)PCI+颈动脉内膜剥脱术:对PCI后择期颈动脉内膜剥脱术的患者维持双抗是合理的,颈动脉内膜剥脱术术后根据情况可适当加用鱼精蛋白。
(3)颈动脉支架+冠脉搭桥:颈动脉支架术前应用抗血小板治疗(阿司匹林,100 mg/d)≥ 2天,冠脉搭桥术后应用低分子肝素抗凝,尽早恢复阿司匹林+ 氯吡格雷≥ 3 个月,阿司匹林终身服用。
8. 围手术期管理要注重两方面,一是抗凝抗栓治疗的衔接,二是严格管理血压、心率。同时还要严格监测心脏和神经系统的症状和特征。
9. 术后降压治疗、心率控制、调脂降糖均需注意。颈动脉血管重建最常用随访评估方法是双功能超声成像,应在术后1、3、6 个月以及此后每年进行监测,以评估再狭窄。必要时可复查CTA或核磁共振血管成像。
10. 冠脉血管重建术后应当定期进行全面的临床和预后评估,包括定期进行心电图、实验室检查、运动试验及超声心动图检测,6~12 个月时建议冠状动脉造影复查。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#颈动脉#
24
#专家共识#
26
更新换代好快啊
37
#冠心病患者#
27
#动脉狭窄#
34
文章好好
53