JAMA Netw Open:2型糖尿病和动脉粥样硬化性心血管疾病患者使用降脂、降压和降糖药物治疗
2022-02-20 从医路漫漫 MedSci原创
根据美国目前的估计,在2型糖尿病和动脉粥样硬化性心血管疾病(ASCVD)患者中,降低心血管风险的循证疗法通常未得到充分应用。
背景:根据美国目前的估计,在2型糖尿病和动脉粥样硬化性心血管疾病(ASCVD)患者中,降低心血管风险的循证疗法通常未得到充分应用。
目的:确定在美国糖尿病和ASCVD患者中使用循证心血管预防治疗。这项多中心队列研究使用了包括12个卫生系统在内的以患者为中心的国家临床研究网络中的卫生系统级汇总数据。设计、设置和参与者:这项多中心队列研究使用了包括12个卫生系统在内的以患者为中心的国家临床研究网络中的卫生系统级汇总数据。参与者包括2018年1月1日至12月31日期间患有糖尿病和已确诊的ASCVD(即冠状动脉疾病、脑血管疾病和外周动脉疾病)的患者。对2020年9月至2021年1月期间的数据进行了分析。
暴露条件:2018年的一次或多次卫生保健情况。
主要成果和措施:患者特征取决于以下任何关键循证治疗的处方:高强度他汀类药物,血管紧张素转换酶抑制剂(ACEI)或血管紧张素受体阻滞剂(ARB)和钠葡萄糖共转运体2抑制剂(SGLT2I)或胰高血糖素样肽-1受体激动剂(GLP-1RA)。
结果:整个队列包括324 706例患者,平均年龄(SD)为68.1(12.2)岁,女性144 169例(44.4%),男性180 537例(55.6%)。共59 124例患者(18.2%)为黑人,41 470例患者(12.8%)为拉丁裔。在前一年的205 885名患者中,17 971名患者(8.7%)就诊于内分泌科,54 330名患者(26.4%)就诊于心脏病科,154 078名患者(74.8%)就诊于初级保健医生。总体而言,190277例(58.6%)患者使用了他汀类药物,但只有88426例(26.8%)患者使用了高强度他汀类药物;14762例(45.5%)患者使用ACEI或ARB, 12724例(3.9%)患者使用GLP-1RA, 8989例(2.8%)患者使用SGLT2I。总体而言,14 918名患者(4.6%)使用了所有3类治疗,138 173名患者(42.6%)没有使用任何治疗。患者开了高强度抑制素更容易被男性(59.9%(95%可信区间,59.6% - -60.3%)的患者和55.6%(95%可信区间,55.4% - -55.8%)的患者),冠状动脉粥样硬化性疾病(79.9%(95%可信区间,79.7% - -80.2%)的患者和73.0%(95%可信区间,72.8% - -73.3%)的患者),更有可能看到心脏病(40.0%(95%可信区间,(39.6% - 40.4%) vs . 26.4% (95% CI, 26.2%-26.6%)。
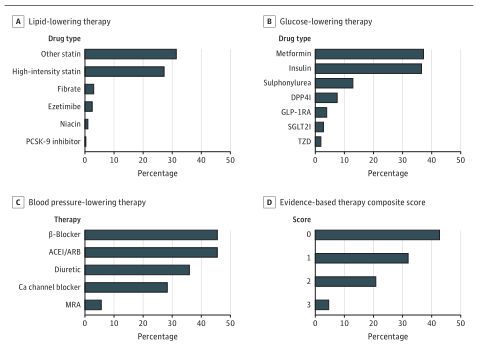
图1接受糖尿病和动脉粥样硬化性心血管疾病循证治疗的患者比例


表1综合循证综合评分的患者特征
结论:在这个美国糖尿病和ASCVD患者的大队列中,不到1 / 20的患者使用了所有3种循证治疗,定义为高强度他汀类药物、ACEI或ARB、SGLT2I和/或GLP-1RA。这些发现表明,需要采取多方面的干预措施来克服实施循证治疗的障碍,督促使用最佳方案。
原文出处:Nelson AJ, O'Brien EC, Kaltenbach LA,et al.Use of Lipid-, Blood Pressure-, and Glucose-Lowering Pharmacotherapy in Patients With Type 2 Diabetes and Atherosclerotic Cardiovascular Disease.JAMA Netw Open 2022 Feb 01;5(2)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
33
#PE#
23
#粥样硬化#
32
#疾病患者#
30
#粥样硬化性#
33
#降糖药#
29
#动脉粥样硬化性心血管疾病#
61
#降压#
37
#降糖药物#
31
#硬化性#
38