Cell Stem Cell:科学家鉴别出饮食压力状态下支持血细胞产生的特殊分子
2018-05-10 佚名 细胞
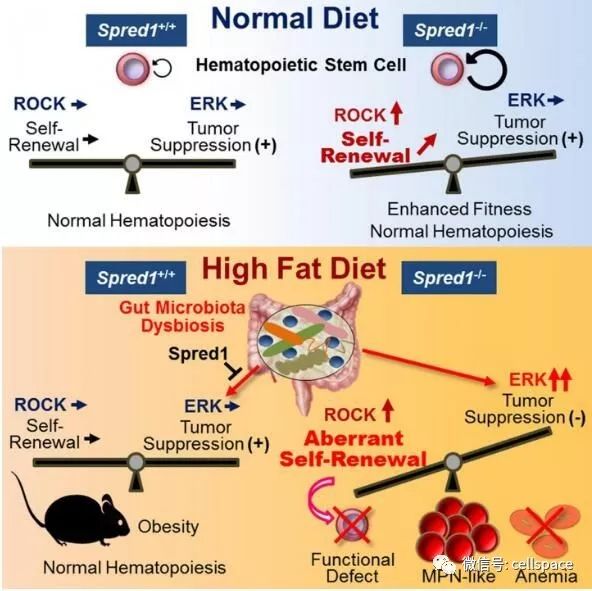
位于骨髓中的造血干细胞(HSCs)能够调节血细胞的产生,当处于特定的压力状况下,比如炎症和衰老,造血干细胞的自我更新能力就会降低,日前,一项刊登于国际杂志Cell Stem Cell上的研究报告中,来自日本金泽大学(Kanazawa University)的科学家们通过研究阐明了Spred1分子在造血干细胞维持动态平衡(自我更新)中所扮演的关键角色,在摄入高脂肪饮食的小鼠体内,Spred1或能保护
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
38
#stem cell#
39
#血细胞#
34
#CEL#
33
#STEM#
31