Blood:miR-185/PAK6轴调控CML耐药性白血病干细胞的存活,可预测治疗反应性
2020-04-18 QQY MedSci原创
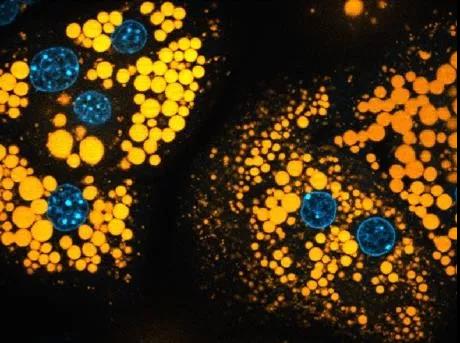
miR-185具有抑癌作用,并可预测未治疗过的CML患者的治疗反应性。 恢复miR-185的表达可影响LSC的存活,使其对治疗敏感;PAK6是miR-185的一个靶基因,介导药物耐受性的发生。
miR-185具有抑癌作用;在体外,恢复其表达可削弱耐药细胞的生存能力,使它们对TKIs敏感,并可显著消除LSCs的长期再增殖和细胞浸润;在临床前异种移植模型中,展现出生存优势。
结合mRNA谱分析发现,PAK6是miR-185的一个关键靶点;药理抑制PAK6可扰乱RAS/MAPK通路和线粒体活性,使治疗耐药细胞对TKIs敏感。
因此,miR-185是一种潜在的预测生物标志物,双重靶向miR85-介导的PAK6活性和BCR-ABL或可为克服患者耐药性提供一种有价值的策略。
原始出处:
Hanyang Lin, et al. The miR-185/PAK6 Axis Predicts Therapy Response and Regulates Survival of Drug-Resistant Leukemic Stem Cells in CML. Blood. April 08, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#白血病干细胞#
48
#PAK6#
31
#反应性#
36
#miR#
35
#miR-185#
42
好
75
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
53
#CML#
52