JAHA:非瓣膜性房颤患者口服抗凝剂类型与痴呆风险的关系
2018-11-05 xing.T MedSci原创
由此可见,服用直接OAC的AF患者痴呆发生率低于华法林服用者。对于与痴呆发生率相关的任何特定直接OAC,没有观察到明显的益处。
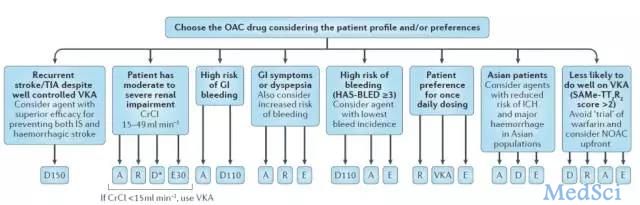
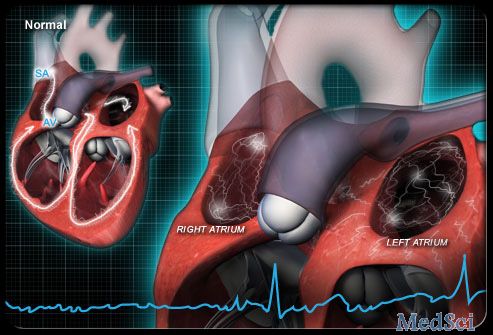
房颤(AF)患者的口服抗凝剂(OACs)除了可降低卒中风险外,还可预防不良的认知结局。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是比较服用不同OAC的AF患者痴呆发生率的风险。
研究人员从MarketScan(2007-2015)和Optum Clinformatics(2009-2015)2个美国医疗索赔数据库中确定了服用OAC的非瓣膜AF患者。痴呆症、合并症和药物治疗情况是根据住院和门诊索赔确定的。研究人员在倾向评分匹配的队列中对华法林、达比加群、利伐沙班和阿哌沙班进行了比较。研究人员计算了每个倾向评分匹配队列和荟萃分析数据库特定结局的事件性痴呆的风险比(HR)和95%置信区间(CI)。
研究人员分析了来自MarketScan数据库的307099例AF患者和来自Optum数据库的161346例患者,其中分别有6572例和4391例患者被诊断为痴呆。每个队列的平均随访时间介于0.7至2.2年之间。服用直接OAC的患者痴呆发生率低于服用华法林患者的痴呆发生率(达比加群:HR为0.85; 95%CI为0.71-1.01;利伐沙班:HR为0.85; 95%CI为0.76-0.94;阿哌沙班:HR为0.80; 95%CI为0.65-0.97)。与直接OAC使用者组相比,痴呆发生率没有差异(达比加群与利伐沙班:HR为1.02; 95%CI为0.79-1.32;达比加群与阿哌沙班:HR为0.92; 95%CI为0.63-1.36;阿哌沙班与利伐沙班:HR为1.01; 95%CI为0.86-1.19)。
由此可见,服用直接OAC的AF患者痴呆发生率低于华法林服用者。对于与痴呆发生率相关的任何特定直接OAC,没有观察到明显的益处。
原始出处:
Nemin Chen.et al.Association of Oral Anticoagulant Type With Risk of Dementia Among Patients With Nonvalvular Atrial Fibrillation.JAHA.2018. https://www.ahajournals.org/doi/10.1161/JAHA.118.009561
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#非瓣膜性房颤患者#
37
#非瓣膜性房颤#
29
#风险的关系#
24
#非瓣膜性#
40
#瓣膜性#
36
#AHA#
22
#口服抗凝剂#
30
#痴呆风险#
24
#瓣膜#
28
#房颤患者#
25