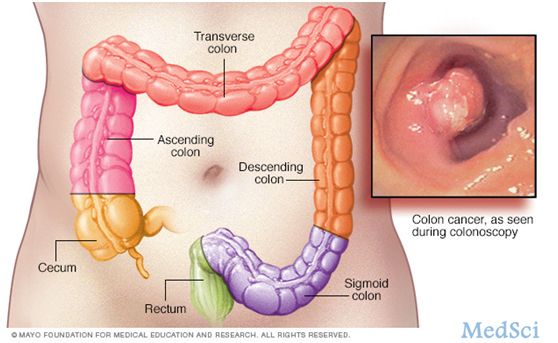
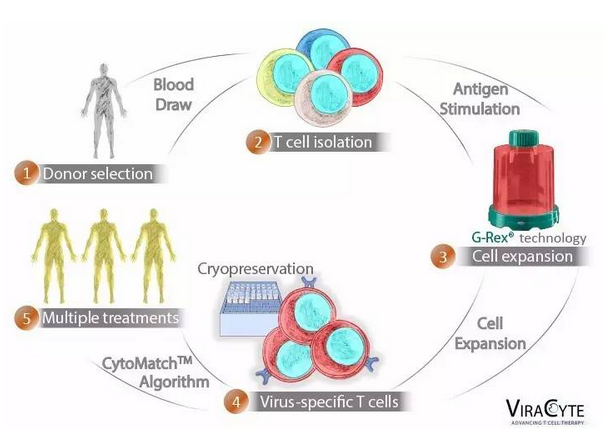
Cell:研究确定癌细胞的“致命弱点”,免疫治疗效果倍增!
2017-09-08 Heather_z727 来宝网
哥伦比亚大学医学中心的一项研究表明,癌症免疫治疗药物只有人受益,但现在用于增加血流量的通用药物可以提高受益几率。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
28
#治疗效果#
28
好文.值得点赞!认真学习了.把经验应用于实践.为患者解除病痛.
49
#CEL#
37
#癌细胞#
32
不错的文章.值得一读
60
学习了.谢谢分享
61
好文.值得点赞!认真学习.应用于实践!谢谢分享给广大同好!
60
到底是cell还是nature?
62