Br J Cancer:粪便免疫化学测试(FIT):结直肠癌低危症状患者的诊断新选择
2021-01-23 xiaozeng MedSci原创
全球每年约有180万新诊断的结直肠癌(CRC)病例以及将近90万例死亡病例。人群筛查可有效的降低患者的死亡率,CRC筛查的相对危险度在0.67至0.88之间,具体取决于筛查形式、筛查频率和性别。
全球每年约有180万新诊断的结直肠癌(CRC)病例以及将近90万例死亡病例。人群筛查可有效的降低患者的死亡率,CRC筛查的相对危险度在0.67至0.88之间,具体取决于筛查形式、筛查频率和性别。
然而,一般筛查到的大多数CRC患者同时也伴随着症状的出现。在英国,只有不到10%的CRC是通过筛查确定的,其余的则是在症状出现后才确定的。在许多国家,有症状的患者首先在初级医疗(社区医疗)服务中就诊,主要由全科医生(GP)评估癌症的可能性, 而在二级医疗服务中的常规诊断检查是结肠镜检查,偶尔使用CT成像或胶囊内镜检查。
粪便免疫化学测试(FIT)是CRC预防的一个好选择,于2017年在英国初级医疗服务中被引入,是一种对潜在的结直肠癌低风险症状的低危患者进行分诊的方法,但目前与基础保健相关的证据很少。
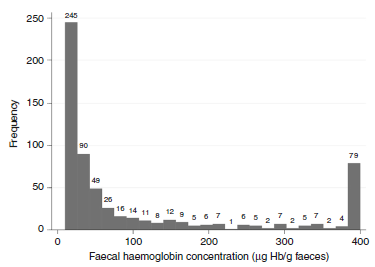
粪便免疫化学定量检测结果直方图
在该研究中,英格兰西南部(人口400万)的所有医疗保健服务提供者均参与了此评估。从2018年6月1日至2018年12月31日,共有3890名年龄≥50岁的就诊患者患有结直肠癌的低风险症状,并接受了一次FIT。粪便诊断的阈值为10μgHb/g,定义为阳性。
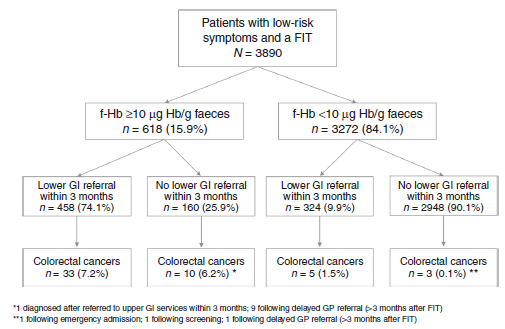
结果显示,618名(15.9%)患者检测为阳性;458名(74.1%)患者在三个月内被紧急转诊至专业的下消化道(GI)服务机构。其中的43名患者在12个月内被诊断出结直肠癌。
FIT检测患者的转诊和诊断流程图
另外的3272患者测试为阴性;324名(9.9%)患者在三个月内有紧急转诊情况发生。在12个月内有8名被诊断出患有结直肠癌。结果显示,阳性预测值为7.0%,阴性预测值为99.8%。敏感性为84.3%,特异性为85.0%。AUC面积(ROC曲线下的面积)为0.92。粪便中37μgHb/g的阈值可识别出个体患癌症风险为3%的患者。
综上,该研究结果显示,FIT在初级医疗服务中对结直肠癌低风险症状的患者进行分类时表现出色。
原始出处:
Bailey, S.E.R., Abel, G.A., Atkins, A. et al. Diagnostic performance of a faecal immunochemical test for patients with low-risk symptoms of colorectal cancer in primary care: an evaluation in the South West of England. Br J Cancer (19 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#FIT#
42
#结直肠#
46
#粪便#
45
好文章,学习了
80