研究发现,对于糖尿病患者来说,他汀是降低冠心病风险的最有效药物。
3月24日,《英国医学杂志(BMJ)》发表的一项Meta分析提示,对于糖尿病患者,在降低非高密度脂蛋白胆固醇(HDL-C)降低方面,在7种常用的他汀中,中高强度剂量(5~40 mg)瑞舒伐他汀、高强度剂量的辛伐他汀(20~40 mg)和阿托伐他汀(40~80 mg)最有效。
而在二级预防人群中,高强度剂量的阿托伐他汀最有效。
与安慰剂相比,中等强度(10~20 mg)阿托伐他汀可显著降低非致死性心梗,降幅为43%。
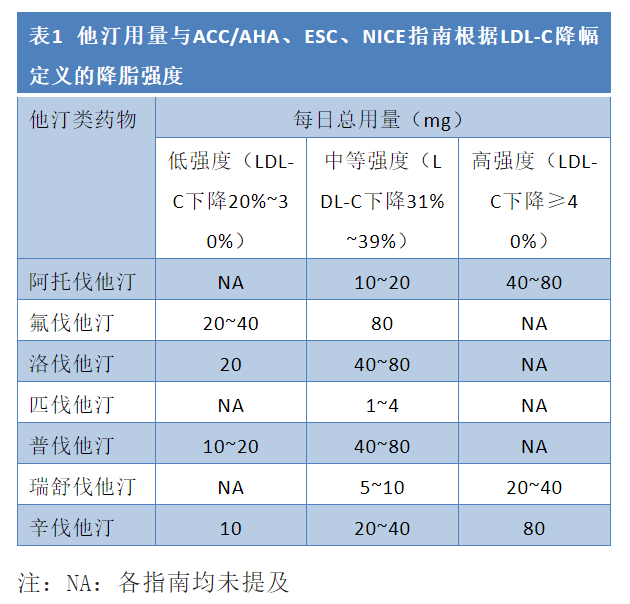
高强度辛伐他汀和瑞舒伐他汀治疗对于降低LDL-C最有效,可将LDL-C水平分别降低1.93 mmol/L和1.76 mmol/L。
作者指出,与LDL-C相比,非HDL-C可更有力地预测心血管病,现在已成为降胆固醇治疗降低心血管风险的主要靶标。该研究对于最有效降低糖尿病患者非HDL-C的他汀类型和强度,提供了指导信息。
研究者共搜集到42项随机对照研究(包括20 193例成年糖尿病患者),最终纳入11 698例患者进行Meta分析。
参考文献:
Comparative effectiveness of statins on non-high density lipoprotein cholesterol in people with diabetes and at risk of cardiovascular disease: systematic review and network meta-analysis. BMJ, 2022, 376: e067731.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Meta#
44
#MET#
43
超级感谢分享
62
#BMJ#
46
#大剂量#
48