肝癌分子靶向治疗面面观:从一线二线治疗决策到综合性全程管理
2019-09-23 佚名 肿瘤资讯
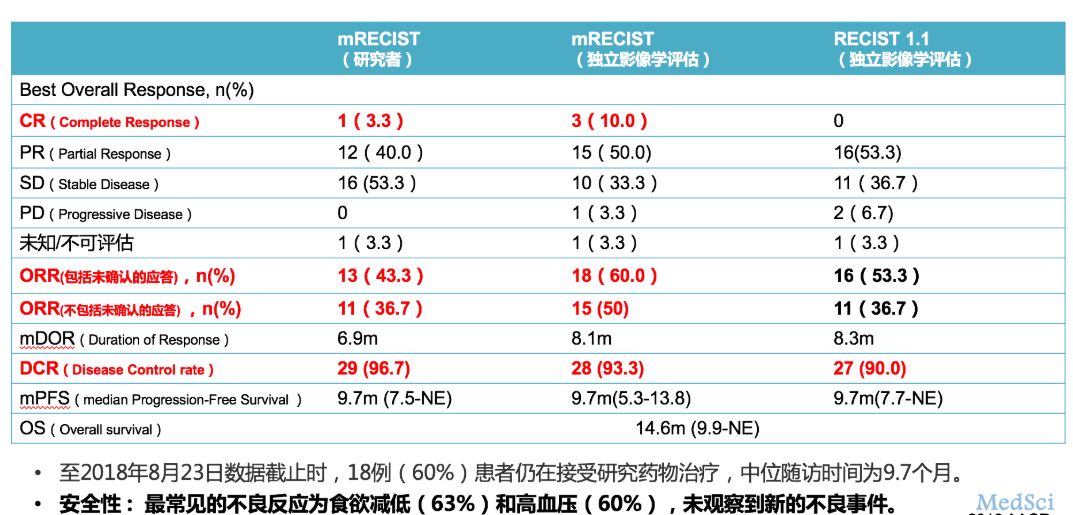
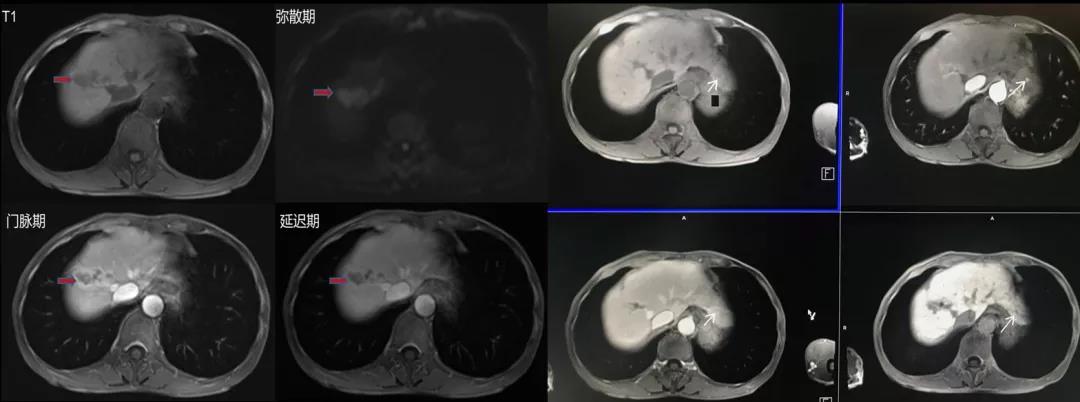
随着医学的进步和技术水平的提高,目前肝癌的治疗已经进入精准治疗和多学科联合治疗的时代。在这一背景下,分子靶向药物在肝癌治疗中的地位如何?一线治疗如何决策?如何对治疗后进展进行评估?肝癌治疗未来将走向何方?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#分子靶向#
44
#全程管理#
47
#治疗决策#
36
#决策#
27
#二线治疗#
24
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
0