当房颤患者遇上新型口服抗凝药,怎么评估怎么用?
2018-06-03 朱文青, CC 医学界心血管频道
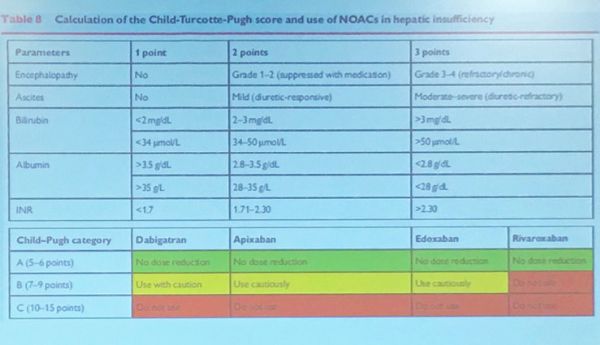
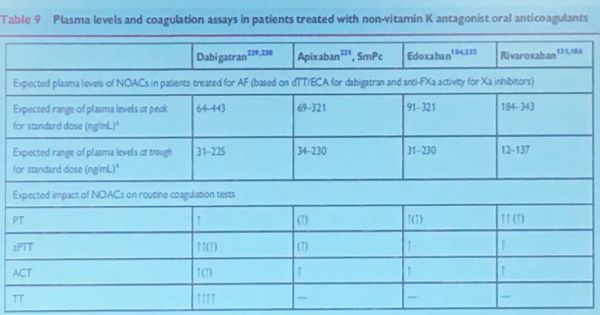
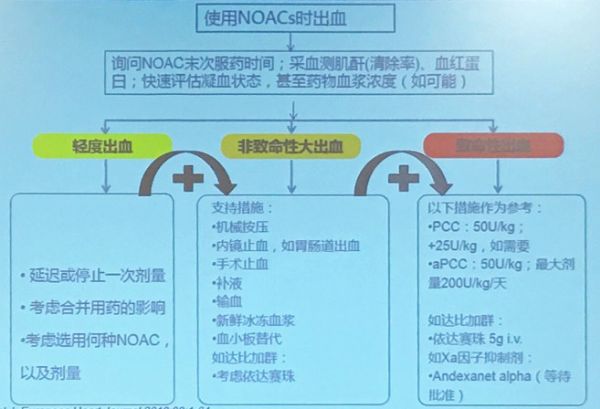
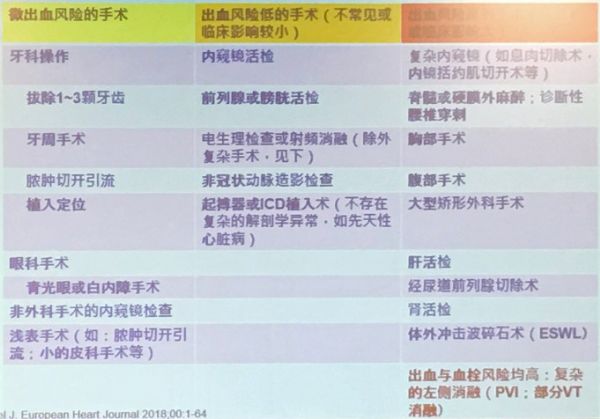
EHRA2018房颤患者新型口服抗凝药(NOACs)临床实践指导更新了,一起来了解一下NOACs的正确使用方法。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新型口服抗凝药#
37
#房颤患者#
30
#口服抗凝药#
30
学习
63
谢谢分享
65
谢谢分享.学习了
65
一起学习学习
2
学习谢谢分享
3
特别实用.感谢作者总结.分享
26
学习了.很实用!
28