CLIN CANCER RES:利用PET检测CD8+T细胞密度
2018-10-29 MedSci MedSci原创
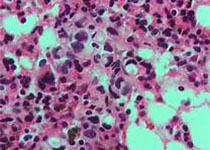
利用PET 对CD8 + T细胞进行无创和定量评估可以用于评估免疫治疗反应。CLIN CANCER RES近期发表了一篇文章,应用标记有64 Cu 的抗CD8 cys-双抗体来评估正常组织和并不组织的PET成像敏感性。
原始出处:
Jai Woong Seo, Richard Tavaré, et al. CD8+
T-Cell Density Imaging with 64Cu-Labeled Cys-Diabody Informs Immunotherapy
Protocols. CLIN CANCER RES. October 2018 doi: 10.1158/1078-0432.CCR-18-0261
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
21
#D8+T#
29
#PET#
26
#CD8#
35
学习了谢谢
1