Eur Respir J:住院患者呼吸困难、死亡率和卫生资源利用之间的关联
2021-03-14 MedSci原创 MedSci原创
任何级别的呼吸困难均与死亡风险增加相关。护理人员可以迅速收集患者呼吸困难的数据,这可能有助于更好地进行监测或采取干预措施,从而降低患者死亡率和发病率。
每10例患者中就有1例在入院时出现呼吸困难,但呼吸困难与患者预后之间的关系尚未明确。
近日,呼吸疾病领域权威杂志Eur Respir J上发表了一篇研究文章,研究人员试图明确入院时呼吸困难是否可以预测患者结局。
研究人员在一个教学医院中心进行了一项回顾性队列研究,分析了67362例连续入院患者的呼吸困难、疼痛和结局数据。在护士进行的初始患者评估中,患者使用0到10的等级(10=难以忍受)对“呼吸不适”进行了评分。患者在入院时报告了呼吸困难,并回忆入院前24小时内经历的呼吸困难。结局包括住院死亡率、2年死亡率、住院时间、需要快速反应系统激活、转移到重症监护室、出院后接受扩展护理以及7天和30天再次入院。
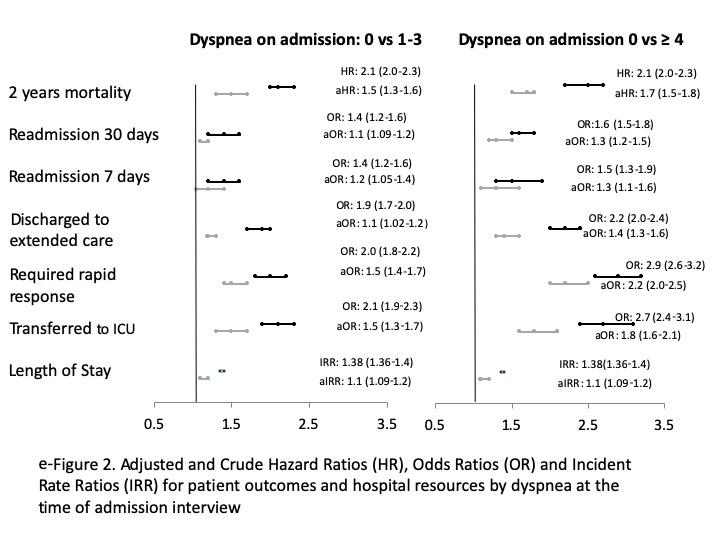
报告有呼吸困难的患者在住院期间死亡的风险增加;呼吸困难程度越严重,死亡风险越大(呼吸困难=0,医院死亡率为0.8%;呼吸困难=1-3,死亡率为2.5%;呼吸困难≥4,死亡率为3.7%,p<0.001)。在对患者合并症、人口统计学和疾病严重性进行调整后,呼吸困难的增加仍与住院患者的死亡率相关(呼吸困难=1-3,aOR为2.1,95%CI为1.7-2.6;呼吸困难=3-4,aOR为3.1,95%CI为2.4-3.9)。疼痛并不能预测增加的死亡率。报告呼吸困难的患者还使用了更多的医院资源,更有可能再次入院,并在2年内死亡风险增加(呼吸困难=1-3,调整后的HR 为1.5,95%CI为1.3-1.6;呼吸困难≥4,调整的HR为1.7、95%CI为1.5-1.8)。
由此可见,任何级别的呼吸困难均与死亡风险增加相关。护理人员可以迅速收集患者呼吸困难的数据,这可能有助于更好地进行监测或采取干预措施,从而降低患者死亡率和发病率。
原始出处:
Jennifer P. Stevens,et al.Association of dyspnea, mortality, and resource use in hospitalised patients.Eur Respir J.2021.https://erj.ersjournals.com/content/early/2021/01/21/13993003.02107-2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#呼吸困难#
35
学习了,谢谢分享
98
高层次研究
87
学习了
87
好文章!
84