Nat Med:华人学者开发新无创产前诊断技术!两大难题一并解决!
2019-01-31 Ruthy 转化医学网
数据显示,除去孕早、中期的流产、胎死宫内以外,约3-5%的出生婴儿存在身体结构或智力缺陷。在所有围产期死亡中,先天性缺陷占20-25%,因此,产前诊断是最大限度免除先天性疾病的道路。
数据显示,除去孕早、中期的流产、胎死宫内以外,约3-5%的出生婴儿存在身体结构或智力缺陷。在所有围产期死亡中,先天性缺陷占20-25%,因此,产前诊断是最大限度免除先天性疾病的道路。近年来,无创产前基因检测技术(NIPS)的问世为广大孕妇免除了有创之苦。但是,NIPS在单基因显性疾病检测方面进展的空白让诸多科学家愁眉不展。近日,贝勒医学院的华人学者张静澜带领的研究团队带来了好消息!他们开发了一项新型NIPS,可以一次性检测30种单基因显性疾病,而且准确率达100%!
NIPS——单基因显性疾病检测,两座大山压顶
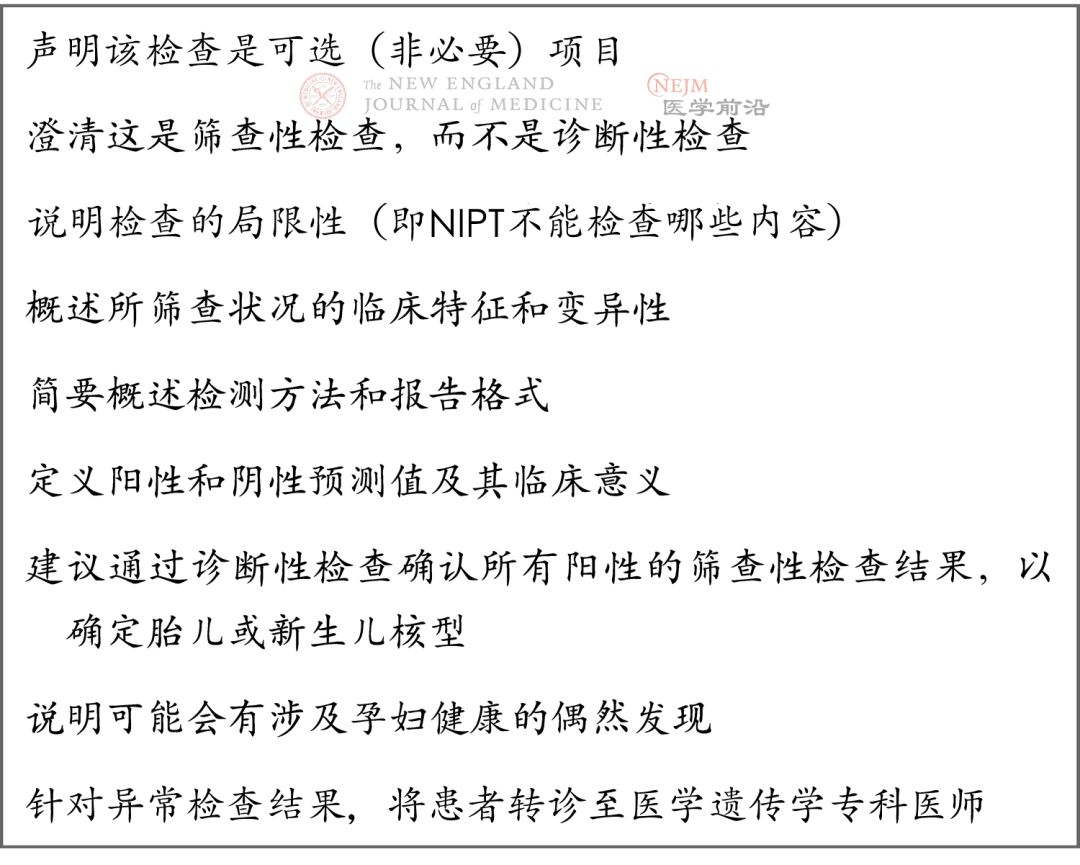
NIPS是近年来产前检测领域出现的一项透过检测血液中游离胎儿DNA的非入侵式产检胎儿染色体疾病检测技术,有效补充了现有的唐氏筛查、羊水穿刺,开辟了产前检测的新篇章,已被证实能降低单基因隐性疾病的筛查成本。但是,其针对单基因显性疾病的筛查却难寻可靠的进展,相关研究屡屡碰壁,这是为什么呢?
难题有二。其一,NIPT是通过NGS技术检测母亲血浆中胎儿的细胞游离DNA(cfDNA)来间接评估胎儿基因状态,相比羊水穿刺等直接的检测手段,这种“间接”的方法利用NGS分析进行建库与测序时极易受到干扰,也就是“噪音”过大。其二,显性突变基因往往存在着大量的假阳性基因,这二者让NIPT对单基因显性疾病的筛查准确率始终难以提高。因此,最大限度地降噪和降低假阳性率就是NIPS应用于单基因显性疾病必须跨过的“两座大山”。
新型NIPS——降噪降假阳性,准确率达100%!
一直以来,NGS时PCR及测序过程中的系统错误造成的假阳性让人们对测序结果不敢全然信任。自2007年开始,陆续有报道指出可用分子条形码(UMI)标记单个模板来解决?NGS?中的?PCR?重复和扩增误差问题。
UMI是将原始样本基因组打断后的每一个片段都加上一段特有的标签序列,用于区分同一样本中成千上万的不同的片段,在后续的数据分析中可以通过这些标签序列来排除由于 DNA 聚合与扩增以及测序过程中所引入的错误。研究人员在NGS分析前期引入UMI,成功对NGS进行有效降噪,使其筛查精度得到显着提高。
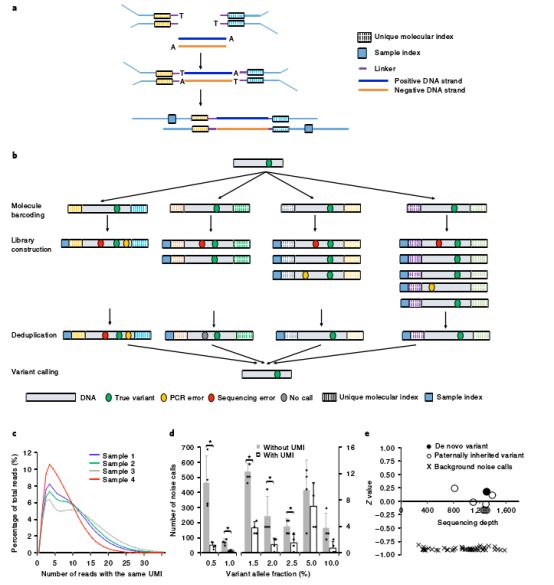
在NGS分析前期引入UMI
而在假阳性基因的筛查方面,研究人员使用存在于母体血浆中胎儿的cfDNA来传递亲本等位基因,并依此开发了基于单核苷酸多态性(SNP)的胎儿分数(FF)计算方法,测试了准确性与灵敏性,最终借此筛查出了假阳性基因。
新型IPNS的高效检测效率
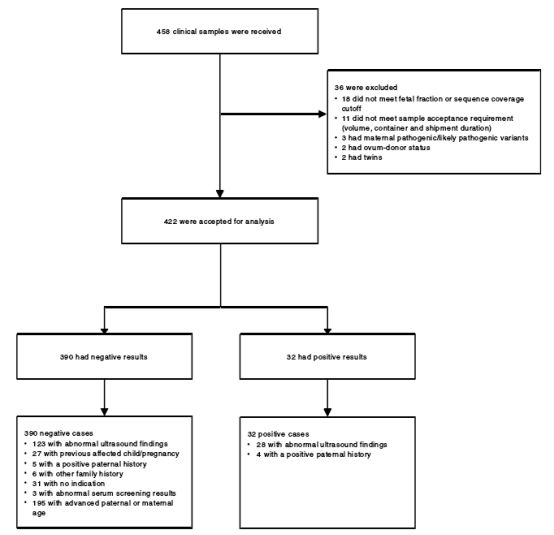
至此,研究团队完美地跨越了IPNS的“两座大山”,而为了验证IPNS技术的精度,便需要大量的样本对技术进行验证。研究人员对458名孕妇进行了30项单基因显性疾病的检测与后续回访。他们利用此项技术一共检测出了35例单基因显性疾病阳性案例,在征得患者同意的20例阳性病例的后续诊断结果中发现所有样本均呈现阳性,这意味着该IPNS技术的检测效率为100%,无任何误差。
这项新型IPNS技术的开发,无疑是为单基因显性疾病的筛查填补了空白。该技术实现了对多种胎儿高发的人类显性单基因疾病的简洁快速准确检测,对进一步评估和管理妊娠有极大的临床价值。
原始出处:Zhang J, Li J, Saucier JB, et al. Non-invasive prenatal sequencing for multiple Mendelian monogenic disorders using circulating cell-free fetal DNA. Nat Med. 2019 Jan 28.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#诊断技术#
0
#Nat#
39
#产前诊断#
34
#产前#
23
#华人#
38
#Med#
20
#华人学者#
49
厉害了我的妹不错,
0
看上去很美
77
感觉很有意义
70