Eur Radiol:肝脏MR弹性成像是否可定量评价门脉高压症?
2021-02-15 shaosai MedSci原创
PHTN可导致许多重要的肝病后遗症,包括与高发病率和死亡率相关的严重静脉曲张出血。因此,早期评估PHTN对改善预后具有重要价值。
门静脉系统压力的病理升高定义为门静脉高压(PHTN),是慢性肝病(CLD)和肝硬化患者并发症的关键驱动因素。PHTN可导致许多重要的肝病后遗症,包括与高发病率和死亡率相关的严重静脉曲张出血。因此,早期评估PHTN对改善预后具有重要价值。肝静脉压梯度(HVPG)的测量目前被作为诊断PHTN的金标准,但由于该方法为侵入性检查,因此在临床上难以常规开展。因此,有必要开发一种非侵入性技术来量化PHTN综合征的门静脉压力。
双参数磁共振弹性成像(MRE)在检测PHTN上是一种很有前途的非侵入性技术。近日,发表在European Radiology杂志的一项研究应用双参数双频MRE预测两种不同小鼠模型的门静脉压力(PP),定量评价PHTN与肝纤维化程度的关系,确定双参数双频MRE预测PP的潜力。
我们研究了73只野生型雄性小鼠,其中包括22只肝充血小鼠,20只胆汁淤积性肝损伤小鼠和31只年龄相匹配的假性对照小鼠。肝剪切硬度(SS)和体积应变(VS)通过在80和200 Hz下的3D MR下获得。 我们在MRE之后立即测量了PP。通过羟脯氨酸法证实肝纤维化。分别使用单频、双频SS和VS拟合广义线性模型来预测PP。通过Spearman的相关性评估预测PP与实际PP之间的关系。 我们用DeLong检验在0.05的显着性水平上比较了所有模型的门脉高压的预测准确性。
患有充血性或胆汁淤积性肝病出现不同程度的明显PHTN和肝纤维化。与假性对照组相比,两种模型中SS显著增加,VS显著减少。所有双参数模型对PHTN均有较高的诊断准确率。双频模型(auc: 0.90[81-95%]、0.91[81-95%])的准确率明显高于单频模型(auc: 0.83[71-91%]、0.78[66-87%])。双频模型预测的PP值与实际PP值的相关性较单频模型更强。
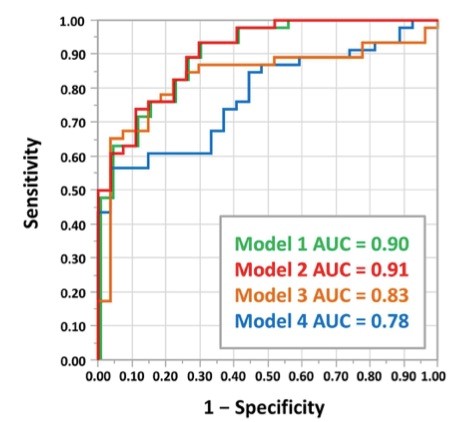
门静脉压力预测模型的ROC曲线
双参数双频模型提高了肝MRE在临床前模型诊断PHTN的准确性。这项技术具有监测不同肝纤维化条件下PHTN的进展和治疗效果的潜力。
原始出处:
Jiahui Li,Tejasav S Sehrawat,Jingbiao Chen,et al. Quantitative assessment of portal hypertension with bi-parametric dual-frequency hepatic MR elastography in mouse models.DOI:10.1007/s00330-020-07341-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#MR弹性成像#
47
#弹性成像#
45
#门脉高压#
38
#评价#
38