体外膜肺氧合联合右心室成型及三尖瓣置换治疗 晚期右心衰竭并发巨大右心房右心室1 例
2019-05-27 许万紫 周庆 曹海龙 心脏杂志
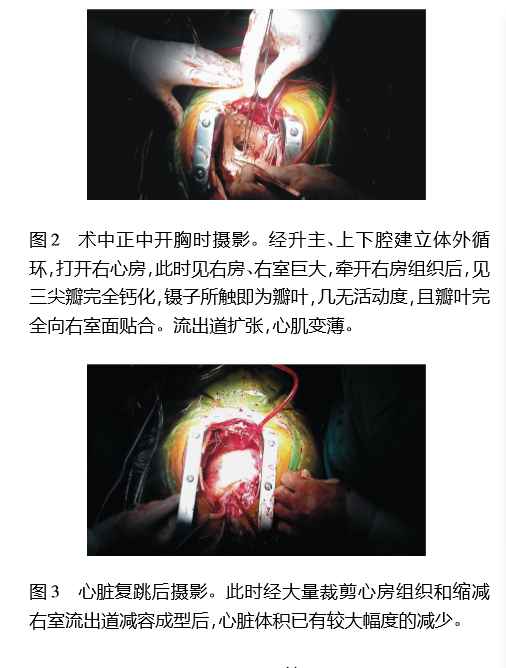
患者女性,66岁,因“反复胸闷气喘伴腹水20余年,加重1周”于2015年8月25日入院。其在20余年前即发现心脏杂音同时并发有心脏扩大,当地医院诊断为扩张性心肌病。长期服用呋塞米、螺内酯、地高辛等进行抗心衰治疗。但于2014年心衰症状进行性加重。并逐渐出现利尿剂抵抗,腹部鼓胀进行性加重,全身恶性消耗(初诊呈四肢纤细腹部胀满的“蜘蛛人”状)。前来我院,完善胸片示心胸比1∶1,见图1,心脏超声示全心扩



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#置换治疗#
34
#右心衰竭#
41
#置换#
26
#并发#
22
#心衰竭#
39
#右心房#
50
#右心衰#
30
#右心室#
24
#三尖瓣#
19
#心房#
20