J Periodontal Res:牙周组织工程中的纤维引导支架
2020-04-15 lishiting MedSci原创
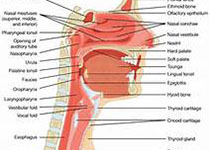
牙周组织为高等级组织器官,它的组成包括牙龈、牙槽骨、牙周膜和牙骨质。牙周炎会导致软硬组织的破坏,最终导致牙齿支持组织丧失。
牙周组织为高等级组织器官,它的组成包括牙龈、牙槽骨、牙周膜和牙骨质。牙周炎会导致软硬组织的破坏,最终导致牙齿支持组织丧失。
常规的治疗能够限制疾病进展;然而,垂直向牙周膜纤维附着于根面牙骨质-真正的再生依旧是一项挑战。已有学者研发了组织工程的方法通过微工程形态特征增加组织再生,特异性的设计能够引导再生膜韧带向牙根表面的插入。这篇综述报告了目前能够产生纤维引导特性的支架制造方法进展,并且阐述了当前这些技术对于形成功能性牙周附着的局限性。
原始出处:
Reuben J Staples, Saso Ivanovski, et al. Fibre Guiding Scaffolds for Periodontal Tissue Engineering. J Periodontal Res., 2020 Mar 5. doi: 10.1111/jre.12729.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
26
#牙周组织#
39
#组织工程#
35
#牙周#
23