Eur Urol:Pembrolizumab+Axitinib与Sunitinib治疗晚期肾细胞癌的生活质量比较
2022-08-25 AlexYang MedSci原创
评估了KEYNOTE-426的健康相关生活质量(HRQoL)情况。
健康相关的生活质量(HRQoL)是衡量癌症患者整体健康状况的一个重要指标。在肾细胞癌(RCC)中,与晚期或转移性疾病有关的症状(疲劳和疼痛)对HRQoL有显著影响。因此,延长无进展生存期(PFS)的治疗可以保留或改善转移性RCC患者的HRQoL,尽管可能因治疗相关的毒性增加症状负担。

既往在3期KEYNOTE-426(NCT02853331)试验中,与Sunitinib单药治疗晚期肾细胞癌(RCC)相比,pembrolizumab + axitinib在总生存期、无进展生存期和客观反应率方面都有改善。
近期,来自德国的研究人员在《Eur Urol》杂志上发表文章,评估了KEYNOTE-426的健康相关生活质量(HRQoL)情况。
研究共纳入了861名患者,并随机分配接受pembrolizumab+axitinib治疗(n=432)或sunitinib治疗(n=429)。429名接受pembrolizumab + axitinib治疗的患者和423名接受sunitinib治疗的患者均有HRQoL数据。HRQoL终点采用欧洲癌症研究和治疗核心组织(EORTC)生活质量问卷(QLQ-C30)、EQ-5D视觉模拟评分表(VAS)和FKSI-DRS调查问卷进行测量。
研究结果发现,在FKSI-DRS(与sunitinib相比改善了-0.79%;95%置信区间[CI]-7.2至5.6)、QLQ-C30(与sunitinib相比改善了7.5%;95%CI 1.0-14)和EQ-5D VAS(与sunitinib相比改善了9.9%;95%CI 3.2-17)调查问卷中,观察到pembrolizumab+axitinib治疗比sunitinib治疗有所改善,但总体改善率没有差异。对于确认恶化的时间(TTcD)和首次恶化的时间(TTfD),在QLQ-C30(TTcD危险比[HR]1.0;95%CI 0.82-1.3;TTfD HR 0.82;95%CI 0.69-0.97)和EQ-5D VAS(TTcD HR 1.1;95%CI 0.87-1.3;TTfD HR 0.98;95%CI 0.83-1.2)中,两组之间无差异。在FKSI-DRS中,TTfD在各治疗组之间没有差异(HR 1.1;95% CI 0.95-1.3),但TTcD在sunitinib治疗组要比pembrolizumab+axitinib治疗更好(HR 1.4;95% CI 1.1-1.7)。
另外,患者在sunitinib非治疗期评估可能会低估sunitinib对HRQoL的负面影响。
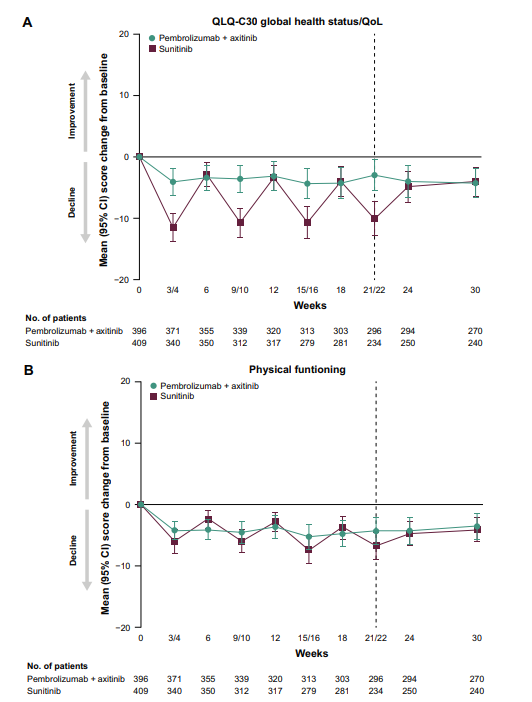
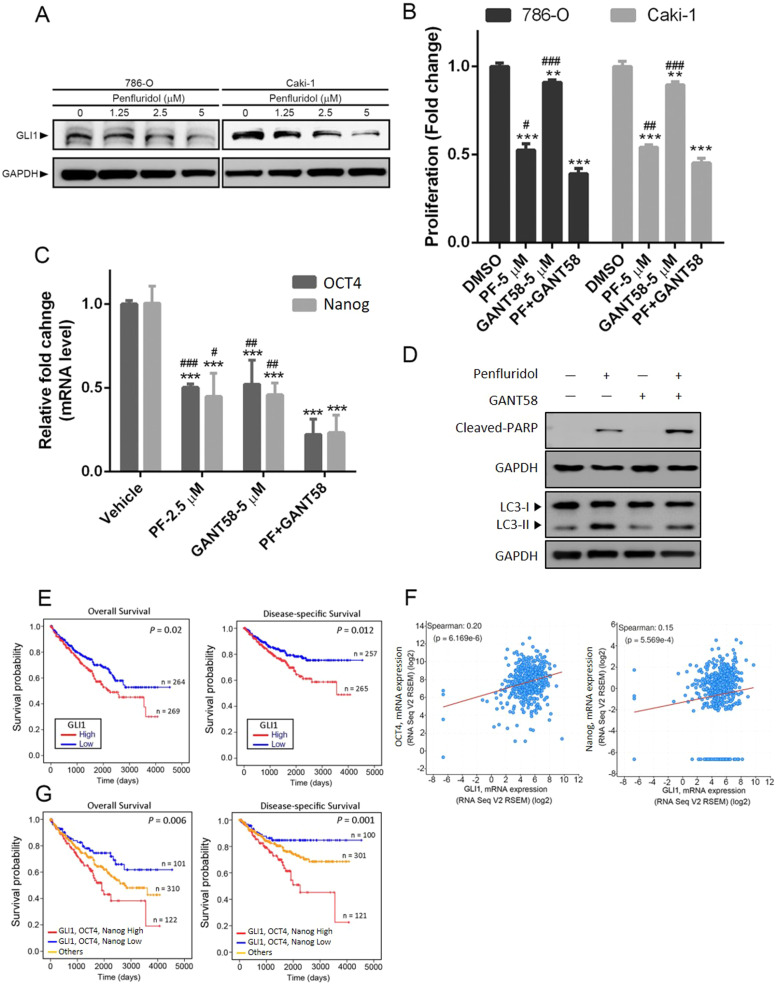
EORTC QLO-C30调查问卷中,相关模块与基线相比的平均变化情况
综上所述,患者报告的结果量表显示,除了FKSI-DRS的TTcD外,pembrolizumab+axitinib和sunitinib两组之间的HRQoL结果没有差异。
原始出处:
Jens Bedke , Brian I Rini , Elizabeth R Plimack et al. Health-related Quality of Life Analysis from KEYNOTE-426: Pembrolizumab plus Axitinib Versus Sunitinib for Advanced Renal Cell Carcinoma. Eur Urol. Jul 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
48
#Pembro#
40
#细胞癌#
41
#mAb#
34
#Pembrolizumab#
47
#晚期肾细胞癌#
39