Science:忘记PD-L1吧,破坏Cdk5也能促进抗肿瘤免疫反应
2016-07-23 生物谷 生物谷
肿瘤通常利用类似于在健康细胞表面上发现的那些蛋白的蛋白进行自我修饰,从而躲避免疫检测。这种防护罩允许它们不被检测地生长,因而经常产生致命性的结果。根据美国脑瘤协会的统计数据,脑瘤每年导致大约1.7万例死亡病例,同时每年新增4600多名儿童脑瘤确诊病例。 通过协调一系列蛋白信号,肿瘤细胞调节它们的防护罩。这些信号通常处于被称作丝氨酸/苏氨酸蛋白激酶的中枢协调蛋白的控制之下。 在一项新的研究中
肿瘤通常利用类似于在健康细胞表面上发现的那些蛋白的蛋白进行自我修饰,从而躲避免疫检测。这种防护罩允许它们不被检测地生长,因而经常产生致命性的结果。根据美国脑瘤协会的统计数据,脑瘤每年导致大约1.7万例死亡病例,同时每年新增4600多名儿童脑瘤确诊病例。
通过协调一系列蛋白信号,肿瘤细胞调节它们的防护罩。这些信号通常处于被称作丝氨酸/苏氨酸蛋白激酶的中枢协调蛋白的控制之下。
在一项新的研究中,来自美国凯斯西储大学医学院的研究人员研究了一种被称作周期蛋白依赖性激酶5(Cdk5)的关卡蛋白,它也是一种在神经细胞和肿瘤细胞发展中起着至关重要的丝氨酸/苏氨酸蛋白激酶。他们特地研究Cdk5在成神经管细胞瘤(medulloblastoma)---一种常见的生长迅速的儿童脑瘤---发展中的作用。他们发现这种关卡蛋白允许某些脑瘤细胞(如成神经管细胞瘤)躲避免疫系统检测。相关研究结果发表在2016年7月22日那期Science期刊上,论文标题为“Cdk5 disruption attenuates tumor PD-L1 expression and promotes antitumor immunity”。论文通信作者为凯斯西储大学医学院儿科学、病理学与生物医学工程副教授Alex Huang博士和儿科学助理教授Agnes Petrosiute博士。
Huang博士解释道,研究人员之所以研究Cdk5,是因为“它大量地表达,而且较高水平的Cdk5与黑色素癌、脑癌、乳腺癌和肺癌患者更差的临床预后相关联。”
当研究人员阻断肿瘤细胞内部的Cdk5并将它们注射回小鼠体内后,一半以上的小鼠存活下来。而在接受仍然含有Cdk5的肿瘤细胞注射的小鼠当中,它们几乎全部都死亡了。这提示着Cdk5在调节小鼠免疫系统对肿瘤作出的反应中发挥着至关重要的作用。通过系统性地剔除这些小鼠体内的一部分白细胞,研究人员能够鉴定出CD4+ T细胞是负责清除缺乏Cdk5的肿瘤细胞和让小鼠远离肿瘤的主要免疫细胞。
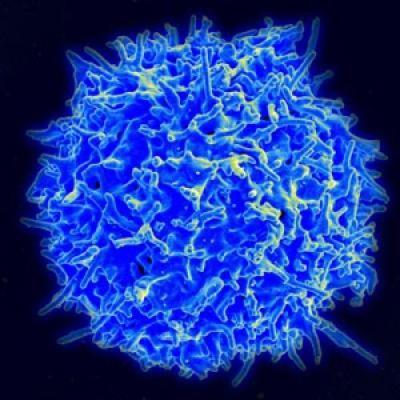
表面上含有CD4分子的人T细胞(即人CD4+ T细胞)部分上通过免疫信号分子干扰素-γ(IFN-γ)进行通信。很多肿瘤细胞通过在它们自己的表面上表达一种被称作程序性细胞死亡配体1(PD-L1)的分子破坏这种通信机制。这种PD-L1蛋白也在免疫细胞表面上发现到,在正常情形下协助“下调”免疫系统活性以便避免免疫反应完成结束后产生附加伤害。表面上表达PD-L1的肿瘤细胞能够类似地让它们的微环境中的T细胞失活,从而逃避免疫系统检测。
研究人员发现肿瘤细胞表面上的PD-L1表达与Cdk5表达相关联。他们测试了几种缺乏Cdk5的肿瘤细胞,结果发现它们不能够在它们自己的表面上强劲地产生PD-L1以作为对免疫信号分子作出的反应。在缺乏Cdk5或PD-L1时,这些肿瘤细胞更容易被免疫系统检测到。他们通过直接破坏肿瘤细胞中的PD-L1基因来证实这一点。在大多数小鼠中,缺乏PD-L1的肿瘤细胞不能够发展为致命性的肿瘤。这些发现清晰地证实Cdk5在调节肿瘤产生PD-L1的能力中发挥着关键性的作用。
Huang说,“我们发现作为一种经常大量表达的蛋白,Cdk5控制着肿瘤细胞如何产生一种重要的关卡分子PD-L1。我们的发现为为靶向Cdk5和相关信号通路的分子疗法作为当前的经常具有严重副作用的疗法的一种替代选择打开大门。”
Cdk5在促进PD-L1表达中所起的关键性作用似乎是高度特异性的。针对免疫信号分子做出反应的其他蛋白并不受肿瘤细胞中的Cdk5缺乏的影响。
除了触发Cdk5在肿瘤细胞表面上表达(和最终促发PD-L1表达)之外,免疫信号分子具有很多功能。研究人员利用几种技术梳理出将免疫信号分子与这些肿瘤蛋白连接在一起的信号通路。他们鉴定出22种蛋白不同程度地受到肿瘤细胞中Cdk5缺乏的影响,其中蛋白IRF2BP2受到的影响最大。这些蛋白可能潜在地作为未来的抗肿瘤药物的治疗靶标。

将近三分之一的肿瘤能够通过阻断PD-L1来加以治疗。这项研究证实阻断Cdk5也可能能够阻断肿瘤表面上的PD-L1和招募CD4+ T细胞来让肿瘤萎缩。研究人员在成神经管细胞瘤中描述了这种信号通路,而且初步的结果提示着它可能也应用于其他的癌症类型中。
根据美国脑瘤协会的统计数据,成神经管细胞瘤大约占所有儿童脑瘤的五分之一。绝大多数的成神经管细胞瘤确诊病例发生于10年以下的儿童体内,而且外科手术摘除是它的主要治疗手段。
原始出处:
R. DIXON DORAND, JOSEPH NTHALE, JAY T. MYERS, DEBORAH S. BARKAUSKAS, STEFANIE AVRIL, STEVEN M. CHIRIELEISON, TEJ K. PAREEK, DEREK W. ABBOTT, DUNCAN S. STEARNS, JOHN J. LETTERIO, ALEX Y. HUANG, AGNE PETROSIUTE.Cdk5 disruption attenuates tumor PD-L1 expression and promotes antitumor immunity. SCIENCE : 399-403
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cdk5#
0
#PD-L1#
27
#免疫反应#
27
#SCIE#
24
#CDK#
23
然而并没有什么卵用,应用,路漫漫啊。
83
科技进步神速
75
了解一下!
112