Diabetes:组蛋白甲基化转移酶MLL1在伤口修复中指导巨噬细胞介导的炎症反应并且其作用在肥胖的2型糖尿病小鼠中发生了改变
2017-07-02 MedSci MedSci原创
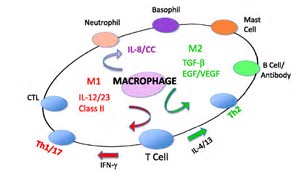
巨噬细胞是伤口修复中发炎期萌生和消除的关键。在糖尿病中,巨噬细胞在后期伤口愈合中表现出持续性的炎症表型。最近发现混合谱系白血病蛋白1(MLL1)通过调控NFκB介导的炎症反应相关基因的转录从而调控基因表达。因此,我们猜测在伤口修复中MLL1会影响巨噬细胞介导的炎症发应。我们利用骨髓特异性Mll1突变体(Mll1f/fLyz2Cre+)探究MLL1在伤口愈合中的功能。与对照相比,Mll1f/fLyz
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BET#
30
#Diabetes#
33
#MLL1#
40
#DIA#
28
#炎症反应#
33
#组蛋白#
26