Hypertension:缺血性卒中住院期间血压波动与3个月临床结局的关系
2022-08-26 MedSci原创 MedSci原创
住院期间较大的血压波动与缺血性卒中发病后3个月不良结局风险增加相关,与平均血压无关。
卒中是全球成年人死亡的主要原因,也是导致长期严重残疾的主要原因。血压升高或高血压是心血管疾病和卒中的主要和可治疗的危险因素。升高的血压变异性与脑小血管疾病、心血管事件和死亡的风险呈正相关。然而,目前还没有大型临床试验证实住院期间血压波动对缺血性卒中临床结局的影响。
近日,心血管权威杂志Hypertension上发表了一篇研究文章,该研究纳入了26家参与医院的3972例急性缺血性卒中患者。研究人员利用住院期间采集的血压数据计算了受试者的血压波动。该研究的主要结局为3个月内死亡或重大残疾的复合结局(改良Rankin量表评分≥3),次要结局包括死亡、血管事件和复合结局(死亡或血管事件)。
与收缩期血压波动的最低四分位数相比,与最高四分位数相关的主要结局调整比值比为1.33(95%CI为1.05-1.68);趋势P=0.011);对于死亡调整后的风险比为2.89(95%CI为1.58-5.32);趋势P<0.001;对于血管事件的调整后的风险比为1.48(95%CI为0.83-2.65);趋势P=0.071;对于复合结局调整后的风险比为2.06(95%CI为1.32-3.23);趋势P<0.001)。
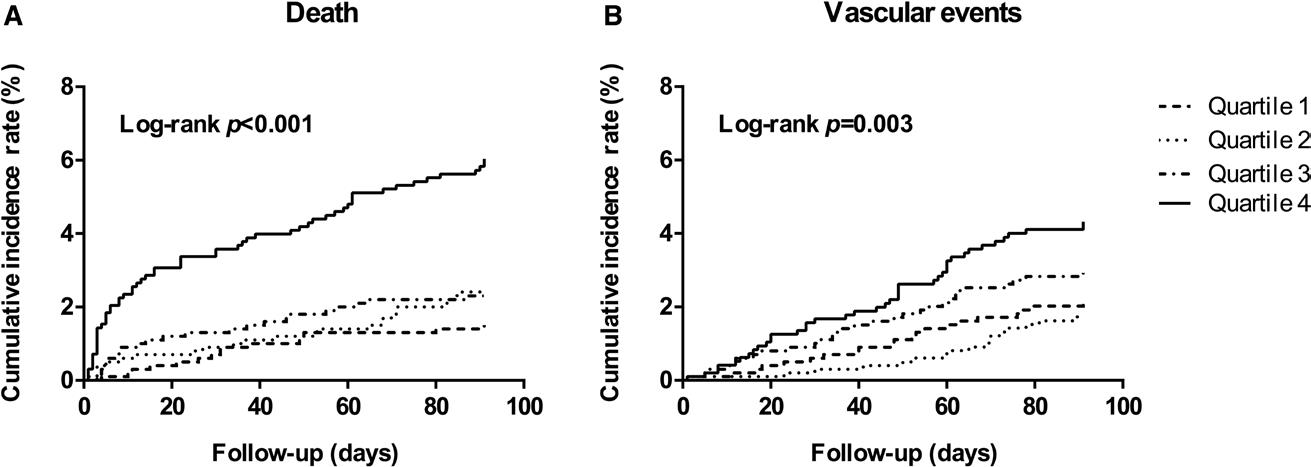
舒张压也有类似的结果。多变量调整限制性三次样条分析显示收缩压波动与主要结局之间存在线性关系(线性P=0.0009)。
由此可见,住院期间较大的血压波动与缺血性卒中发病后3个月不良结局风险增加相关,与平均血压无关。这些结果提示血压波动可能是缺血性卒中不良结局的危险因素,这些结果为血压管理策略提供了新的思路。
原始出处:
Ruirui Wang.et al.Blood Pressure Fluctuation During Hospitalization and Clinical Outcomes Within 3 Months After Ischemic Stroke.Hypertension.2022.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.122.19629
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TENS#
53
#缺血性卒#
46
#临床结局#
55
#血压波动#
41
#PE#
38
#缺血性#
0
#Hypertension#
43