Acta Physiologica: 消炎药能抑制肌肉生长
2017-08-29 MedSci MedSci原创
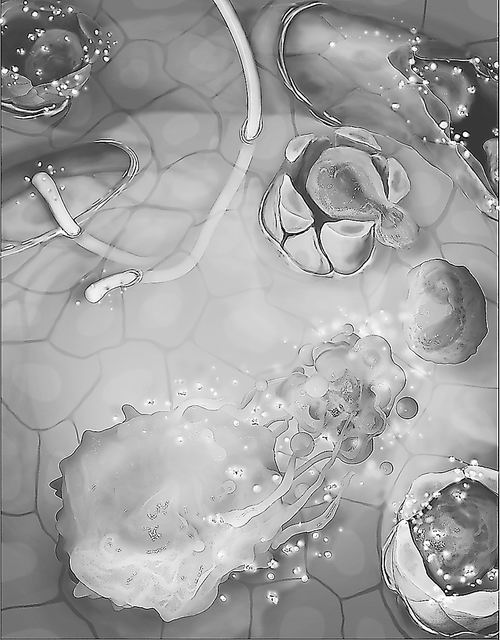
根据卡罗林斯卡学院的一项新的研究,进行重量训练的年轻、健康人群若长期使用非处方抗炎药,会抑制肌肉的增长。并报道了布洛芬对骨骼肌的影响,研究发表在Acta Physiologica上。除扑热息痛之外,大多数解热镇痛的非处方药都是NSAID(非甾体类抗炎药)。这些药物是世界上被广泛使用的药物,它们都能抑制所谓的COX酶。在本研究中,18至35岁的健康男性和女性被随机分为两组,一组每天服用较高剂量的NS
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#肌肉生长#
32
#CTA#
39
#Physio#
49
#消炎药#
35
好东西学习了!
68
超厉害的说.有点意思
70