经十二指肠镜行逆行胰胆管造影术后感染及防控策略现状
2017-01-03 《中华医学杂志》 《中华医学杂志》
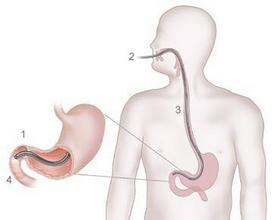
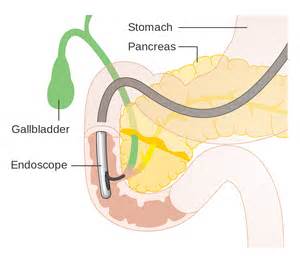
目前经内镜逆行胰胆管造影术(endoscopic retrograde cholangiopancreatography,ERCP)是临床处理胆膜疾病的重要手段,如今诊断性ERCP已逐步发展为治疗性ERCP。ERCP是一项具有一定风险的侵入性操作,与操作有关的并发症并不罕见,胆道感染是常见的并发症之一。尤其是2015年美国特大耐药大肠杆菌爆发感染事件更将十二指肠镜清洗消毒质量控制的重要性提升到
目前经内镜逆行胰胆管造影术(endoscopic retrograde cholangiopancreatography,ERCP)是临床处理胆膜疾病的重要手段,如今诊断性ERCP已逐步发展为治疗性ERCP。ERCP是一项具有一定风险的侵入性操作,与操作有关的并发症并不罕见,胆道感染是常见的并发症之一。尤其是2015年美国特大耐药大肠杆菌爆发感染事件更将十二指肠镜清洗消毒质量控制的重要性提升到历史高度。如何减少通过十二指肠 镜进行ERCP检查和治疗导致的相关胆道感染并发症的发生,确保患者安全,需要一系列有效的质控方法和防控措施。
一、ERCP术后感染的现状
1.国外ERCP术后感染现状:有研究指出,在不同的人群中ERCP术后胆道感染的发生率从2.2%到21%不等。近几年,十二指肠镜诊疗后发生的多重耐药菌爆发相关报道屡见不鲜。2013年伊利诺伊州9例多重耐药菌感染患者中有6例(66.7%)有ERCP手术史。2014年宾夕法尼亚州一家三级教学医学中心发生一系列内镜相关抗碳青霉烯类肠杆囷属(carbapenem-resistantenterobacteriaceae,CRE)感染患者腹腔内实质性器官的感染发生,并在十二指肠镜中培养出耐碳青霉烯克雷伯菌,18例细菌培养阳性患者中有9例有ERCP手术史,且感染细菌为同一菌种。
2.我国ERCP术后感染现状:国内的一项研究指出587例次ERCP术后患者中,并发胆道感染120例次,感染率为20.4%;120例胆道感染患者中,死亡6例,均死于急性化脓性胆管炎合并多脏器衰竭。我国目前罕见超级细菌交叉感染的报道。
3.内镜相关感染对患者安全性的影响:由于可重复使用设备的清洗、消毒不彻底而致传染性物质的转移造成的伤害是非常严重的。2014年和2015年美国医疗机构关注的患者安全十大问题中包括了器械消毒,特别指出内镜和手术器械的清洗、消毒不当。
二、ERCP术后感染的危险因素
不同研究报道ERCP术后感染发生率不同,但对ERCP术后胆道感染确切的危险因素均不清楚,现主要从十二指肠自身特点和清洗消毒质量、ERCP操作技术相关因素和非技术相关因素进行分析如下:
1.十二指肠镜清洗消毒相关因素
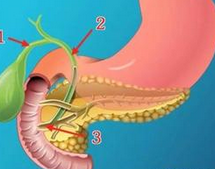
(1)十二指肠镜材质的特殊性:消化内镜是一种重复性使用的诊断和治疗器械,构造精细,管腔复杂,材料特殊,不易清洗,不适于高温高压消毒,多数采用化学消毒剂浸泡消毒或灭菌。按照斯波尔丁分类系统,十二指肠镜属于中危险度应进行高水平消毒。不幸的是,目前还没有证实的解决方案可以彻底消除十二指肠镜相关微生物污染的风险。例如,对于胃肠道(GI)内镜如十二指肠镜,没有低温灭菌技术能够达到106的无菌保证水平(SAL)。
(2)十二指肠镜构造的特殊性:十二指肠镜构造的自身特点更是增加了清洗消毒的难度,内镜活检钳道是ERCP治疗所需器械、配件等辅助工具通过的管道,很容易有细菌存留,并且该部分也很难清洗。在大多数因内镜检查而发生的感染事件中,最后都在活检钳道内部找到了相应的病原菌。此外,十二指肠镜独有的通道用来定位导管、指引导丝和附件进入内镜视野,这个独立的通道设计复杂且存在缺陷,导致清洗刷很难进入刷洗,从而影响内镜的清洗消毒再处理效果。
(3)十二指肠镜清洗消毒过程及质量控制:①内镜清洗消毒流程执行不完整:国内外均有颁布实施内镜清洗消毒指南和相关法规,美国CDC文献建议严格遵守这些指南才能确保内镜消毒安全。不幸的是,进一步的数据显示,内镜手工清洗消毒相关的所有步骤很少被执行,一些必须的步骤(例如刷洗所有的腔道和部件)一般情况下都没有落实,导致内镜的清洗消毒效果难以保证。②内镜清洗消毒设备不 完善:使用不恰当的再处理设备,如与十二指肠镜不匹配的活检钳道清洗刷、不是专门的清洗刷,均会导致清洗不彻底,影响十二指镜的消毒质量。
2.ERCP操作中技术相关因素
(1)ERCP操作人员的技术水平:ERCP操作人员的技术水平与ERCP术后并发症的发生有直接关系,有研究指出反复插管可损伤胆管并影响0ddi括约肌功能,继而引起胆道感染。注入过多造影剂或操作中患者恶心、呕吐致胆管内形成一种往返性、灌注式的高压可引起肠胆反流,这也可能增加术后胆道感染的发生率。国外一项前瞻性研究发现,ERCP操作全程时间是术后发生胆道感染的危险因素之一。
(2)医源性感染:在行ERCP过程中,难以做到绝对无菌操作,外源性的细菌很容易在胆管内繁殖并通过肝血窦进入门静脉系统造成严重的感染。
(3)ERCP操作过程及治疗手段:据报道,胆汁引流不充分、胆管恶性肿瘤、十二指肠乳头切开和支架置入是ERCP术后胆管炎发生的相关因素。
3.ERCP操作中非技术相关因素
(1)胆道梗阻部位及性质:ERCP术后胆道感染的发生与胆管梗阻的性质和部位有关。国内有研究报道,ERCP术后并发胆道感染与恶性梗阻性黄疸及靠近肝门部梗阻密切相关,梗阻原因中恶性胆道梗阻发生率最高(65.0%),梗阻部位又以肝门部发生率最高(81.8%),其次为肝总管(42.4%)和胆总管(18.2%)。
(2)其他病变:国内有文献指出伴有其他一些病变的患者接受ERCP治疗时也易并发胆道感染,如原发性硬化性胆管炎、十二指肠乳头旁憩室、胆管囊性扩张症、肝移植术后、胆囊切除术后及全身免疫功能低下等。
三、十二指肠镜感染的防控策略
1.十二指肠镜清洗消毒质量改善
(1)十二指肠镜抬钳器的正确清洗:如果使用钳道可进入的十二指肠镜,那么手工预清洗过程中的冲洗和刷洗、清洗消毒机中钳道的正确连接和终末彻底干燥都是至关重要的。可拆卸的头端帽和先端部使得预清洗变得更容易,因为清洗刷能轻松伸进抬钳器中进行刷洗,但是在再次使用之前,需要仔细地重新安装好这些可拆卸的部分。
(2)避免“超说明书”的做法:固定的先端部在预清洗过程中要求更加精确,因为日常的清洁刷很难进入内镜钳道后面狭窄的内腔进行清洁。需要使用专用的清洗刷,且这些都不应造成内镜任何损伤。为了避免“超说明书”的做法,制造商(内镜或者清洁配件的制造商)应当提供对清洗设备兼容性的相关数据。
(3)床侧预清洗和手工预清洗:内镜拔出后,要立即进行床侧预清洗,使用蘸有多酶清洗液的纱布或一次性多酶清洗液湿巾将内镜表面擦拭干净,避免分泌物干燥后难以清除。来回按下送气送水按钮至少10s、间断吸引空气和多酶清洗液,并将按钮取下,刷洗干净后,放到多酶清洗液内进行超声震荡清洗。摘除十二指肠镜插入部的前端帽,使用十二指肠镜专用毛刷进行刷洗,然后连接抬钳器,控制钢丝管道口,用多酶清洗液进行冲洗和浸泡。即使使用了自动化的再处理,彻底的手工预清洗仍然必不可少。因为这是达到理想消毒效果的前提条件。工作人员应当意识到这一步骤的重要性。任何偏离指南和操作规程的行为都可能导致再处理过程的失败。
2.内镜清洗消毒效果质量监控:日常的技术测试和微生物监测可评估结果的质量,并且是早期识别任何问题、缺陷和薄弱环节的有用工具。美国相关机构对暴发事件做出回应并发布了十二指肠镜微生物监测的临时建议,建议中不包括内镜所有的附件和通道。欧洲指南推荐每3个月进行一次常规的微生物监测,并强调需要对内镜所有的附件和可用的通道进行采样。在已发表的各种论文中,监测频率和检测 流程仍是争议的焦点问题,尚需进一步的研究。一旦存在污染,临床工作人员应停用可疑的仪器设备,直到采取了校正措施并且达到了满意的结果方可重新使用。
3.人员培训:美国和欧洲在继超级细菌感染爆发事件后,提出了改善内镜清洗质量的一揽子策略,其中都强调了内镜清洗消毒人员培训的重要性。因为医疗器械的再处理要求操作人员应具备专业的知识及技能,只有受过专业培训的和能胜任此工作的人员才能进行内镜的再处理。许多国家已经建立了内镜再处理的正式培训课程和评估胜任能力的系统。医生、内镜护士和内镜清洗消毒人员应当意识到他们担负着患者安全的责任。如果不严格遵循国家指南和本机构操作规程,感染的潜在风险就会增加。对再处理过程定期检查、定期开展相关培训和进行能力评估都是工作中有用的工具,帮助我们识别工作中的缺陷、执行改进措施和确保及时更新操作方法。
4.严格无菌操作:提高ERCP术操作水平,术中严格坚持无菌原则以减少胆道感染的发生。操作前要铺设无菌操作台,操作人员插管前更换无菌手套,尽量使用一次性配件,如果使用复用配件要确保已经经过清洗灭菌。操作中也要具备无菌观念,如多个研究报道,在十二指肠乳头插管前、胆管造影前使用无菌生理盐水冲洗活检钳道和配件可以降低ERCP术后胆管感染的发生率。同时,定期进行治疗室的空气培养和仪器设备物体表面消毒效果监测,并做好医疗废弃物的整理与回收工作,最大限度降低ERCP术后感染的发生。
5.治疗性ERCP应彻底胆道减压、充分引流:正常情况下胆道系统具有防御机制,当疾病、手术或ERCP操作破环胆道系统对感染的防御机制,就会并发ERCP术后胆管炎的发生。无论何种原因引起的胆道梗阻,均可造成胆汁引流不畅,胆汁淤积是造成胆道感染的重要原因之一。操作者应该依照患者的病情进行胆管内引流术或胆管外引流术,使胆道引流通畅,可以减少胆道感染的发生率。
6.预防应用抗生素:对于ERCP术前预防性使用抗生素的问题尚无定论。国内和国外的文献均表明非选择性预防应用抗生素不能有效防止ERCP术后胆管炎发生,因此不推荐常规预防应用抗生素。但是对于引流不充分等特殊患者 需预防应用抗生素。
总之,随着ERCP技术日益普及,其已成为胆胰疾病治疗中不可取代的手段,而ERCP术后胆道感染问题也越来越被关注,但只要严格遵照内镜清洗消毒法规和内镜清洗消毒指南是可以确保内镜安全的。在操作过程中注意无菌操作、 提高人员的操作水平等一系列有效预防措施,可以减低ERCP术后感染的发生。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#造影术#
42
#十二指肠镜#
39
#十二指肠#
26
#防控策略#
33
#肠镜#
23
#造影#
27
#胆管#
27