抑郁症会导致心肌梗死后的恢复变得复杂且缓慢,也会对个人的精神面貌、人际关系和生活情趣造成影响。第71届美国心脏病学会科学年会(ACC.22)上将公布的一项旨在评估心肌梗死后的抑郁患病率和卒中发生率趋势的研究显示,与没有抑郁症的群体相比,心肌梗死后患有抑郁症的群体发生卒中的可能性高出约50%。
该研究分析了美国近50万心肌梗死发作患者的健康记录,这项有史以来研究抑郁症与心肌梗死之间关系的规模最大的研究之一发现,在健康状况和人口统计学背景相似的抑郁症患者和非抑郁症患者中,卒中发生率存在显着差异。
研究人员使用Trinetx数据库分析了2015年-2021年期间495,386名心脏病患者的健康记录。Trinetx将来自全美58个医疗系统的电子医疗记录数据汇集到一个基于云的单一服务中,研究人员可以在保护患者隐私和安全的同时分析多个数据来源。共有51000名患者(10.5%)在心肌梗死发作后被诊断为抑郁症。
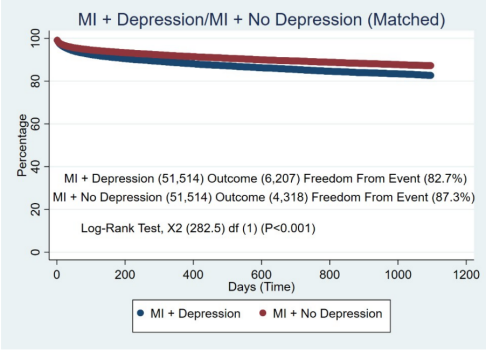
在这些患者中,大约六分之一的人在心肌梗死发作之前就被诊断出精神健康障碍,而其他人则是在心肌梗死发作后首次被诊断出抑郁症。研究人员将51000名抑郁症患者与同一数据集中没有抑郁症的其他心脏病发作幸存者进行了比较发现,12%的抑郁症患者和8.3%的非抑郁症患者随后患上卒中,卒中风险相差近50%。

该研究主要作者,西弗吉尼亚州查尔斯顿地区医疗中心心脏病学部门的Frank H. Annie博士表示,这两个队列之间的唯一区别就是有无抑郁症,可能有很多与抑郁相关的因素导致了这些结果。例如,患有抑郁症可能会干扰一个人预约就诊和药物治疗依从性的能力。抑郁症还会干扰睡眠和注意力,使定期锻炼和保持心脏健康饮食变得具有挑战性。男性比女性更容易患抑郁症。患有抑郁症的人也往往有较高的高血压、冠状动脉疾病、糖尿病、心力衰竭和慢性阻塞性肺病发病率,以及较高的体重指数和吸烟史。然而,即使在考虑了这些变量之后,抑郁症和随后卒中之间的关联仍然显着。
既往研究已经指出抑郁症和心肌梗死之间的联系。虽然这种关系所涉及的确切原因和影响仍不清楚,但越来越多的证据表明,接受抑郁症治疗可以帮助改善心肌梗死患者的预后。在这项研究中,只有7%的抑郁症患者使用过抗抑郁药。需要进一步的研究来了解抑郁症和其他因素是如何影响心脏健康和卒中及其他形式的心脏病风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#卒中风险#
45
#临床实践#
46
#ACC#
55
学习
58