J Clin Oncol:戈舍瑞林和他莫西芬辅助治疗绝经前乳腺癌患者的长期益处
2022-08-01 MedSci原创 MedSci原创
雌激素受体阳性的绝经前患者采用内分泌辅助治疗2年,获益最长可达20年
绝经前乳腺癌患者罹患致命性疾病的风险增加。由于这些患者是在生命早期被诊断出来的,因此长期风险和治疗益处对这个患者群体特别重要。
Stockholm试验旨在评估绝经前乳腺癌患者的长期(20 年)内分泌治疗益处。本文对该试验进行了二次分析。
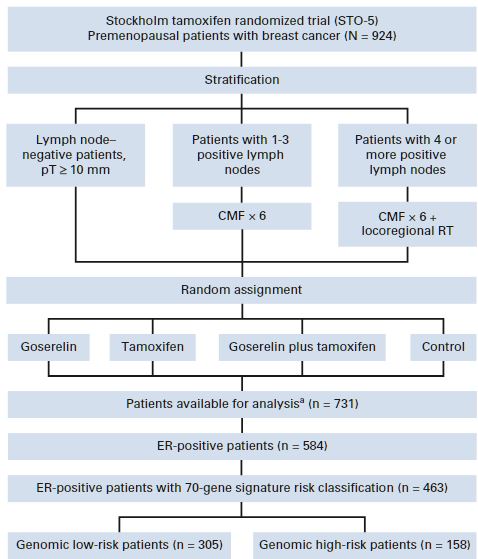
在该试验中,924位绝经前患者被随机分组,予以两年的戈舍瑞林(3.6 mg,皮下注射,1次/28天)、他莫西芬(40 mg/日,口服)、戈舍瑞林+他莫西芬或非辅助内分泌疗法(对照)。并按淋巴结状态将患者分层,淋巴结阳性患者(n=459)被分至标准化疗组(环磷酰胺、甲氨蝶呤和氟尿嘧啶)。
研究流程
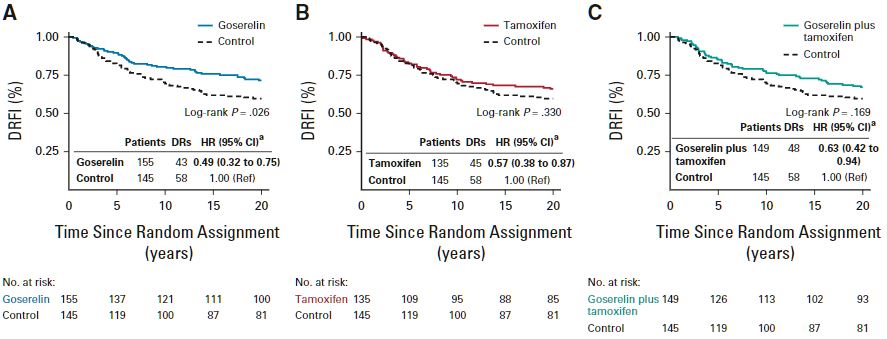
在激素受体阳性患者(n=584,中位年龄47岁)中,对对照组相比,戈舍瑞林、他莫西芬和戈舍瑞林+他莫西芬均可显著改善长期无远处复发间隔(多变量风险比[HR] 0.49;HR 0.57;HR 0.63)。研究人员观察到戈舍瑞林与他莫西芬之间存在显著的相互作用(p=0.016)。
各组的长期无远处复发间隔
基因组低风险患者(n=305)显著受益于他莫西芬(HR 0.24),基因组高风险患者(n=158)可从戈舍瑞林中显著获益(HR 0.24)。基因组高危患者,采用戈舍瑞林+他莫西芬治疗的风险会增加(HR 3.36)。此外,在基因组低风险患者中观察到了他莫西芬治疗的长期益处(20年),而基因组高风险患者采用戈舍瑞林治疗有较显著的早期获益。
总之,该研究显示,雌激素受体阳性的绝经前患者采用内分泌辅助治疗2年,获益最长可达20年,而且肿瘤基因组特征不同的患者可从不同的方案中获益。戈舍瑞林联合他莫西芬相比单用任一药物没有显著益处。
原始出处:
Annelie Johansson, et al. Twenty-Year Benefit From Adjuvant Goserelin and Tamoxifen in Premenopausal Patients With Breast Cancer in a Controlled Randomized Clinical Trial. J Clin Oncol. July 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.02844
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
56
#绝经前#
49
#戈舍瑞林#
39
#绝经#
48
#他莫西芬#
54
#乳腺癌患者#
43