Acta Haematologica: 新生儿脐带血的正常值和独特的形态学特征
2021-11-21 MedSci原创 MedSci原创
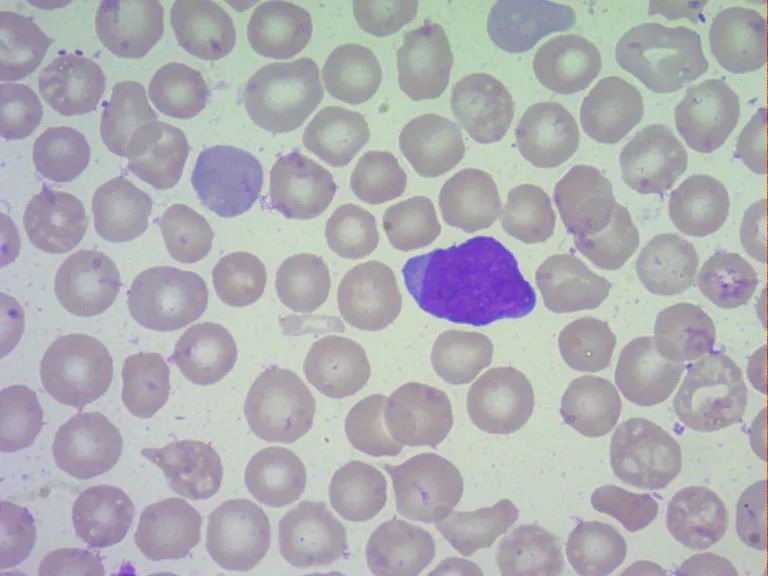
本研究描述了新生儿CB的正常值和独特的形态学特征。CB中丰富的形态异常淋巴细胞可能代表出生时免疫系统的不成熟状态。
脐带血(CB)一直是研究和各种临床应用的宝贵造血干细胞来源,也可用于诊断新生儿的各种疾病和状况。CB 细胞成分的一些参数可以由自动分析仪提供,而其他参数,如未成熟或异常细胞,需要血膜形态评估。以往的研究表明,CB中的白细胞群可能与正常外周血(PB)不同,不仅存在未成熟细胞,而且还存在其他类型的细胞。例如,自然杀伤(NK)细胞在PB和CB中分别占淋巴细胞的10%和30%。国外进行一研究,目的是建立正常的 CB 形态,并确定 CB 中形态异常白细胞的患病率。

对取自健康母亲所生的健康足月和适当胎龄新生儿、早产新生儿、糖尿病母亲的新生儿和小于胎龄新生儿的 100 个 CB 样本进行了全面的形态学分析。采集时间为1年,100例CB样本分别来自54名男性和46名女性新生儿。评估血细胞计数,并由实验室专家进行人工形态学分析。100个CB样本中有12个来自患有以下疾病的母亲所生的新生儿:甲状腺功能减退症,产后,妊娠期间巨细胞病毒感染,母亲治疗选择性5 -羟色胺再摄取抑制剂,分娩期间抗生素治疗,所有病例都很少(少于5例),其中3例无法进一步分析。因此将这12个样本排除在进一步分析之外。
图1:脐带血(CB)样本的血液学评估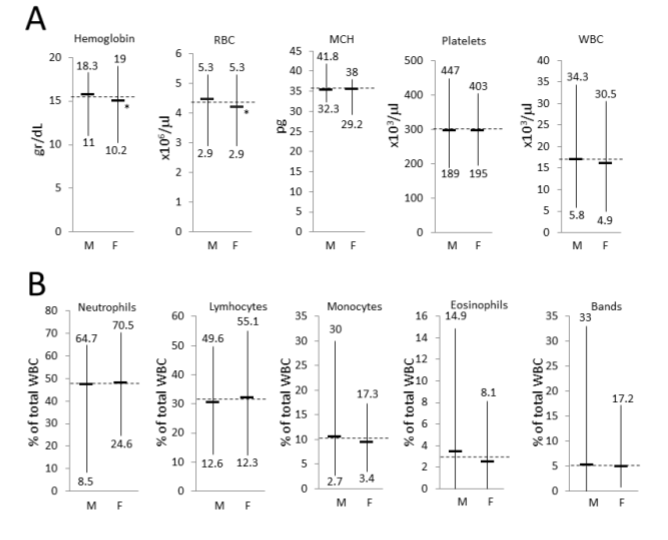
图2: 淋巴细胞亚型的形态学评估

图3:脐带血样本按新生儿状态分类。88份脐带血样本根据不同的新生儿状态进行分组(A-F)分析,见表(右)。左:每组中样品出生体重、胎龄和APGAR5的平均标准差

结果显示正常CB标本手工差示计数:中性粒细胞47.8±10.7%,淋巴细胞31.2±9.8%,单核细胞10.0±4.0%,嗜酸性粒细胞3.0±2.5%,性别差异无统计学意义。在 44/100 个样品中观察到爆炸,每个样品平均为 0.5±0.7%,并且仅观察到轻微的左移。无论新生儿状态如何,样本中都存在大量大颗粒淋巴细胞(占淋巴细胞总数的 19.1±10.6%)和形态异常的淋巴细胞(占淋巴细胞总数的 12.4±5.4%)。早产 CB 样本与正常足月 CB 样本的差异显着,包括中性粒细胞/淋巴细胞比率的逆转和嗜碱性粒细胞的缺乏。
图4:根据新生儿状态区分主要类型白细胞计数。
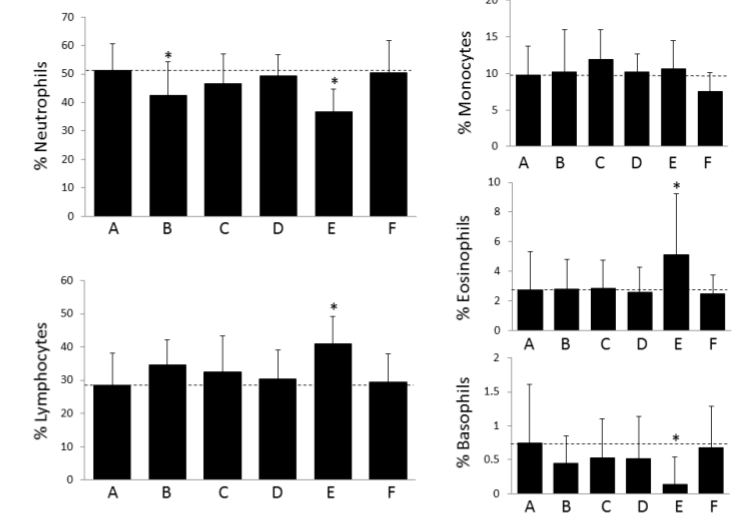
图5: 根据新生儿状态区分淋巴细胞亚型计数。
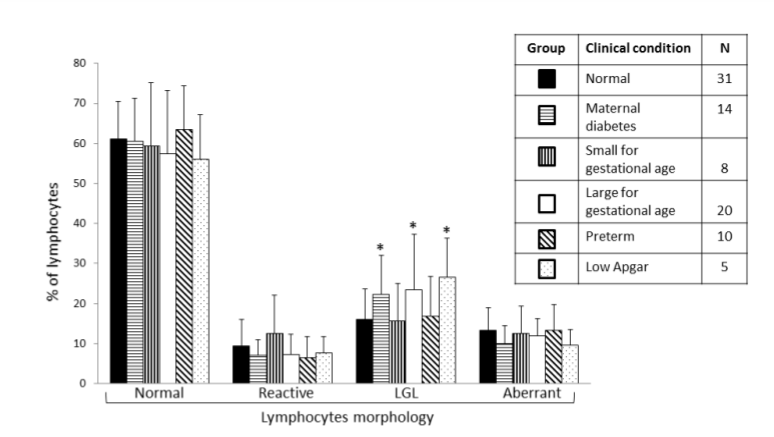
图6:脐带血样本红细胞形态分析

总的来说,本研究描述了新生儿CB的正常值和独特的形态学特征。CB中丰富的形态异常淋巴细胞可能代表出生时免疫系统的不成熟状态。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#HAE#
42
#CTA#
39
#EMA#
35
#脐带血#
38
#脐带#
52
学习了
50
学习了!!!
51