Blood:巨噬细胞TNF-α纵容供体T细胞合成IFN-γ促进骨髓衰竭
2018-10-26 MedSci MedSci原创
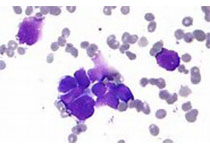
中心点:宿主巨噬细胞来源的TNF-α和供体T细胞上表达的TNF-αR在小鼠免疫介导的骨髓(BM)衰竭的病理机制中发挥重要作用。再生障碍性贫血(AA)患者BM中合成TNF-α的CD16+CD68+巨噬细胞的量要高于健康供体的。摘要:一直以来都认为干扰素-γ(IFN-γ)和肿瘤坏死因子-α(TNF-α)参与再生障碍性贫血和其他骨髓衰竭综合征的免疫病理生理,但具体机制尚未完全明确。近期,有研究人员在小鼠
宿主巨噬细胞来源的TNF-α和供体T细胞上表达的TNF-αR在小鼠免疫介导的骨髓(BM)衰竭的病理机制中发挥重要作用。
再生障碍性贫血(AA)患者BM中合成TNF-α的CD16+CD68+巨噬细胞的量要高于健康供体的。
摘要:
一直以来都认为干扰素-γ(IFN-γ)和肿瘤坏死因子-α(TNF-α)参与再生障碍性贫血和其他骨髓衰竭综合征的免疫病理生理,但具体机制尚未完全明确。近期,有研究人员在小鼠免疫介导的BM衰竭模型中明确了供体T细胞所产生的IFN-γ和宿主的IFN-γ受体的基本功能。研究人员利用他们的小鼠模型和具有INF-α或INF-α受体(TNF-αR)基因缺陷的小鼠模拟了类似的机制。出人意料,将INF-α-/-的供体淋巴结(LN)细胞输注到CByB6F1受体或将FVB的LN细胞输注到TNF-αR-/-受体小鼠中,均可诱导骨髓衰竭,同时,小鼠血浆的IFN-γ和TNF-α水平均显著升高。
此外,在TNF-α-/-受体小鼠中,骨髓损伤被缓解,提示宿主器官的TNF-α对免疫破坏造血作用必不可少。在注射LN前敲除宿主巨噬细胞可减弱T细胞IFN-γ的水平,并减轻骨髓损伤,而给输注了FVB-LN细胞的INF-α-/-受体小鼠再输注重组TNF-α可增加T细胞IFN-γ的表达,,并加速骨髓损伤。
除此之外,将TNF-αR-/-供体的LN细胞输注到CByB6F1受体小鼠可减轻骨髓T细胞浸润、抑制T细胞产生IFN-γ,并减轻骨髓损伤。
综上所述,宿主巨噬细胞来源的TNF-α和供体T细胞上表达的TNF-αR对小鼠免疫介导的骨髓衰竭的病理生理至关重要,通过调节IFN-γ的分泌发挥作用。对于AA患者,骨髓中产生TNF-α的巨噬细胞要多于健康供体,提示TNF-α/IFN-γ和巨噬细胞均参其病理过程。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#供体#
26
#骨髓衰竭#
49
#TNF#
21
#IFN#
32