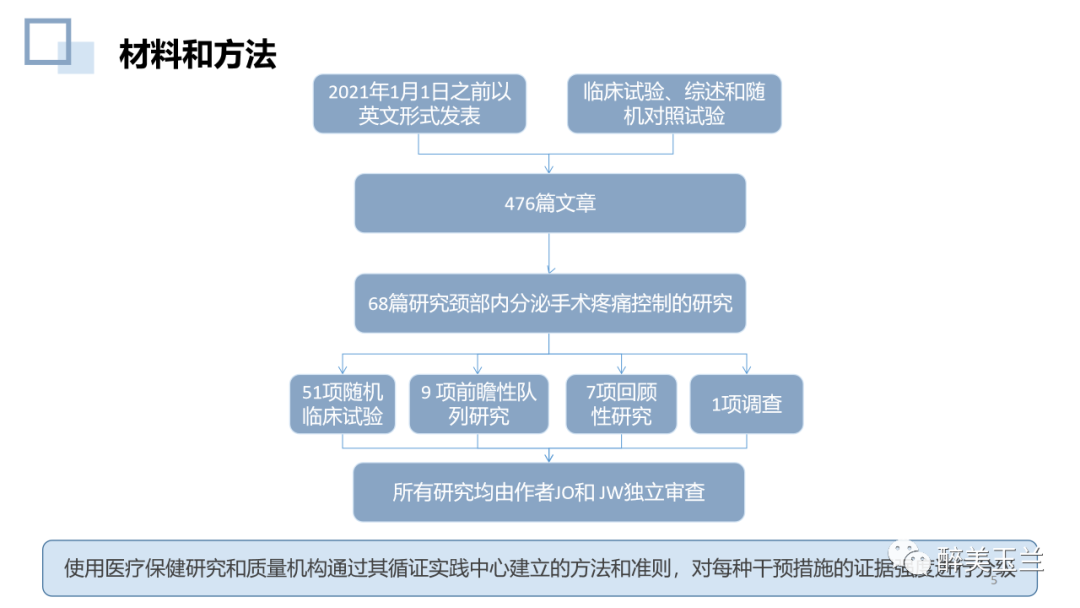
文献学习:甲状腺和甲状旁腺手术的围手术期疼痛管理:系统综述
2022-02-28 醉美玉兰 醉美玉兰
美国每年进行超过15万例甲状腺手术和11万例甲状旁腺手术,5%至7% (大约每年19000 名)接受此类手术且首次使用阿片类药物的患者在手术后3-6个月仍会继续使用麻醉镇痛药。
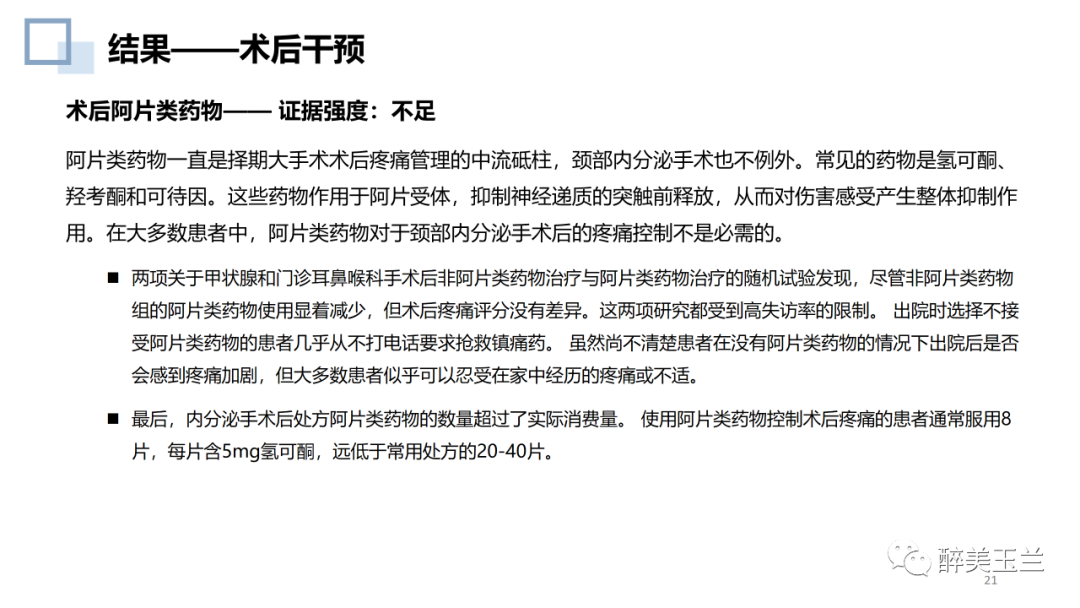
美国每年进行超过15万例甲状腺手术和11万例甲状旁腺手术,5%至7% (大约每年19000 名)接受此类手术且首次使用阿片类药物的患者在手术后3-6个月仍会继续使用麻醉镇痛药。目前,关于颈部手术后阿片类药物的镇痛模式和非麻醉性辅助药物的使用,在临床实践中存在着很大的差异。
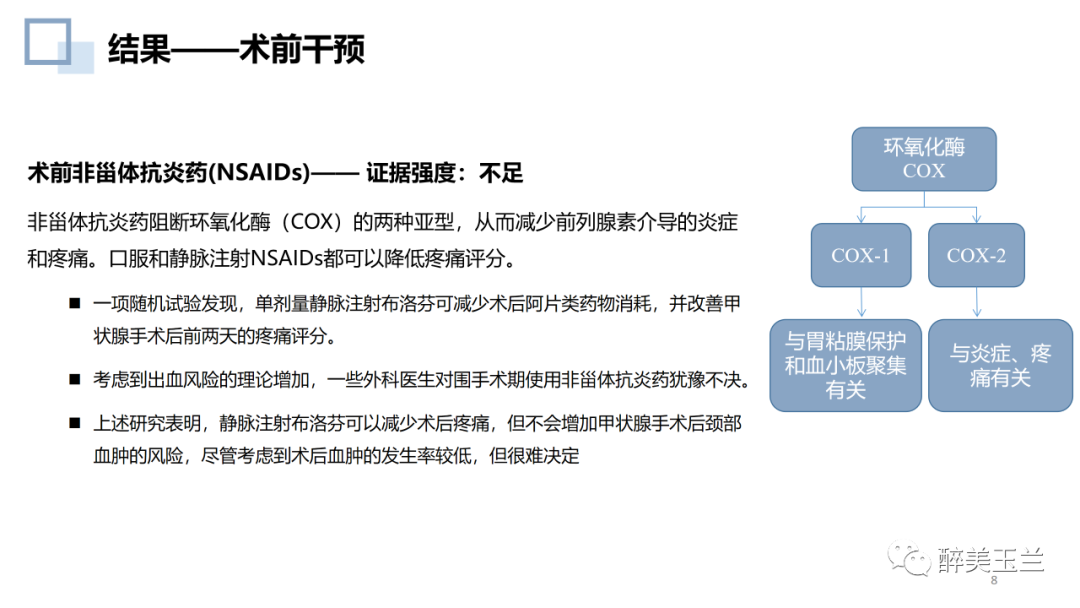
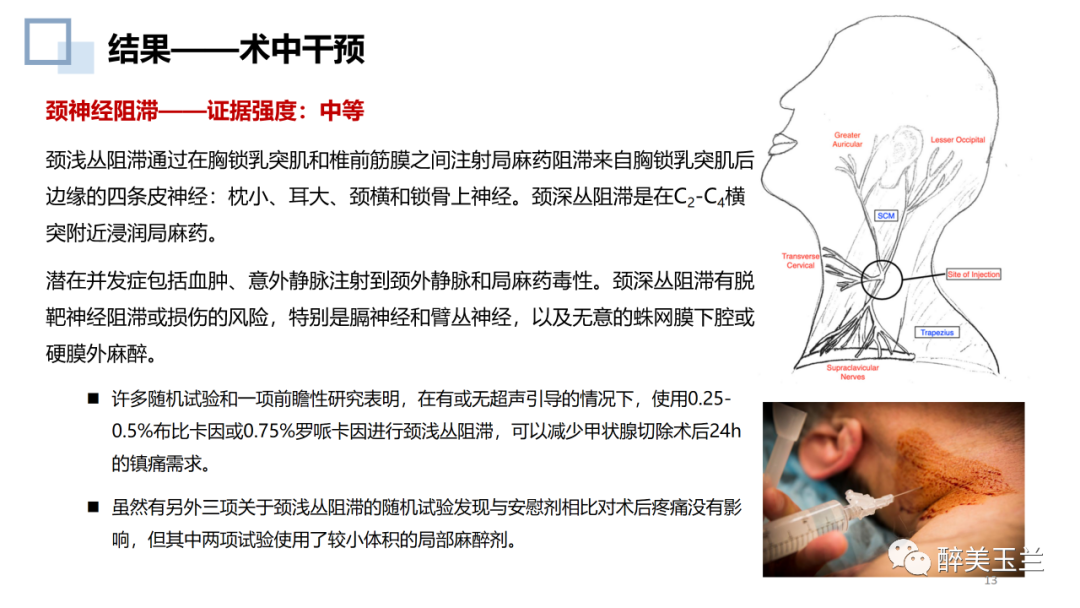
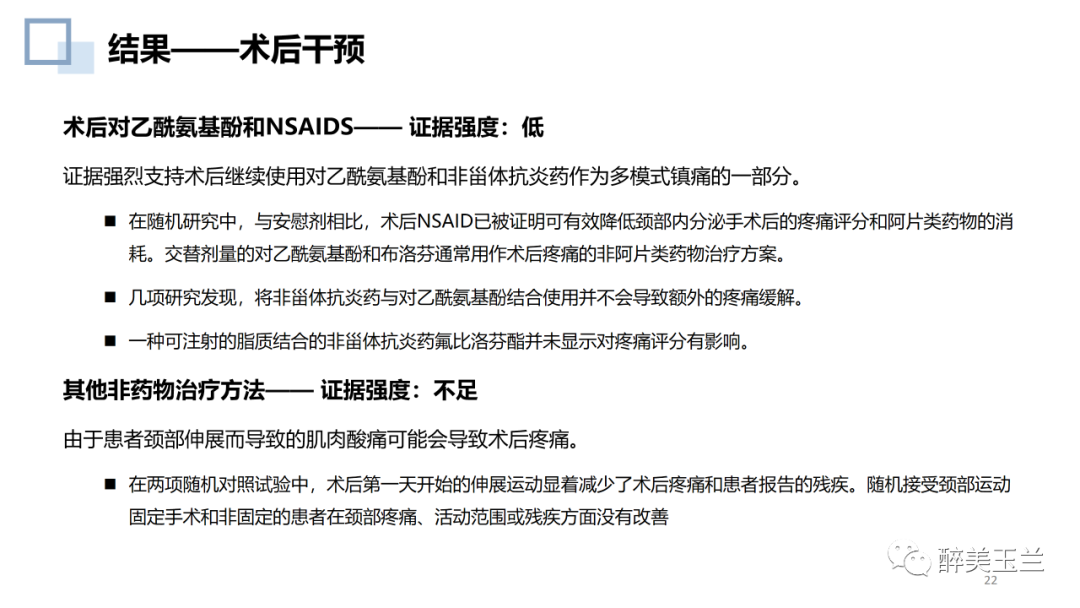
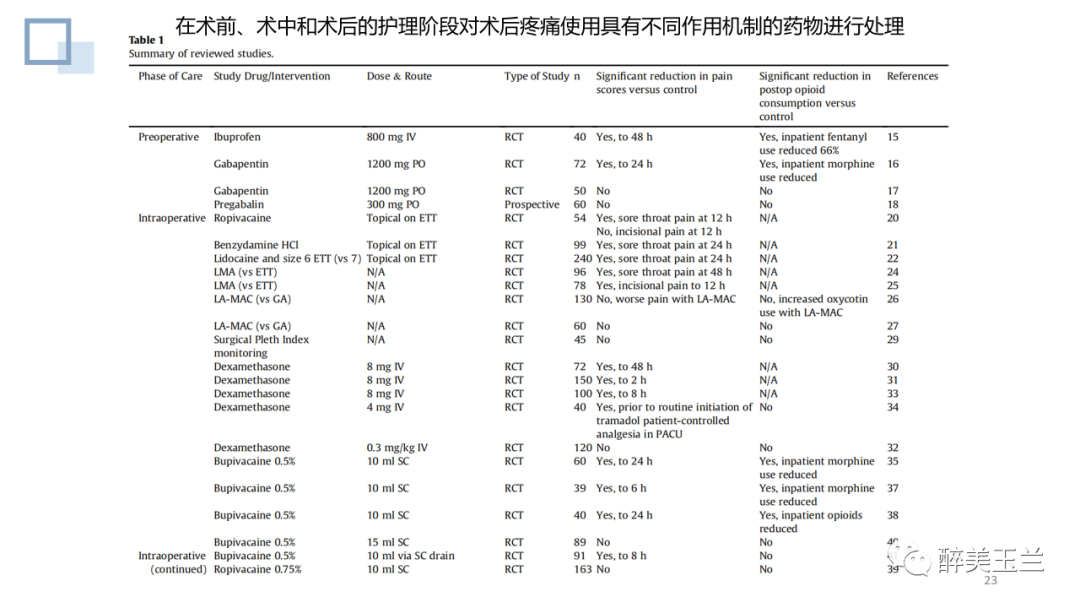
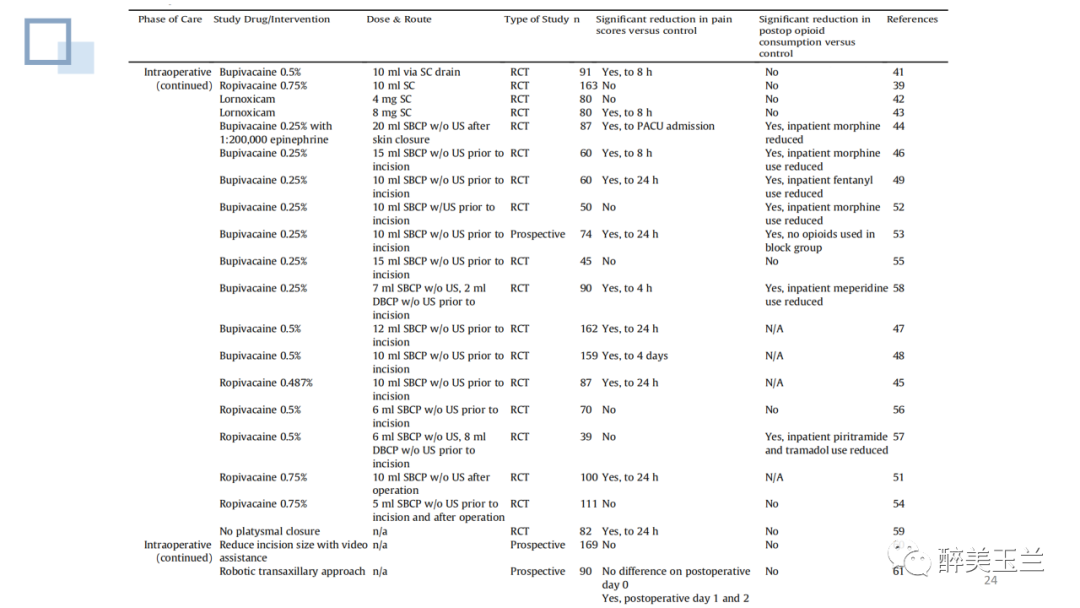
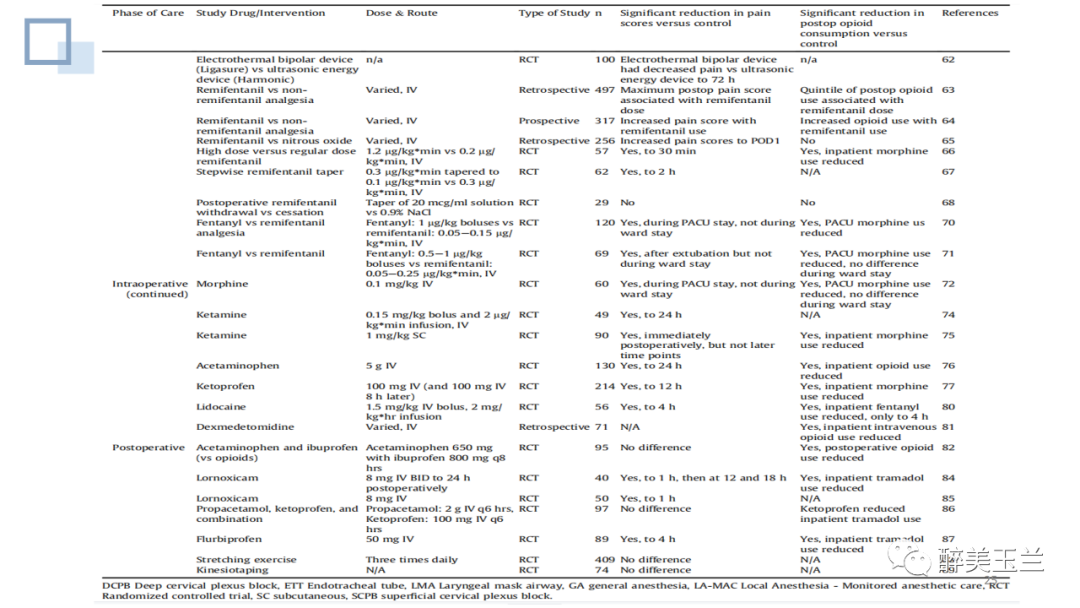
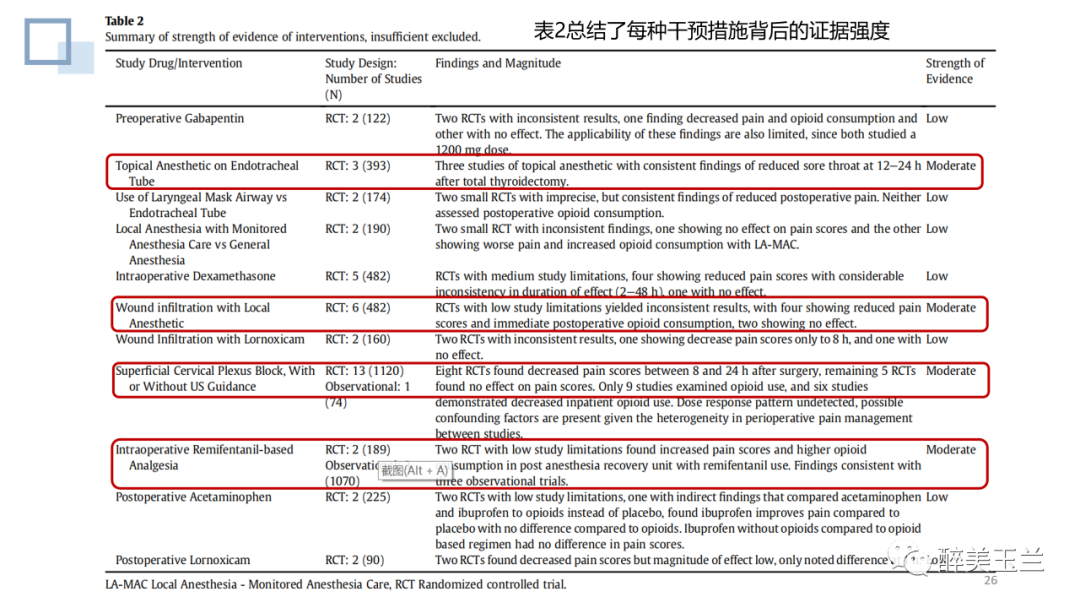
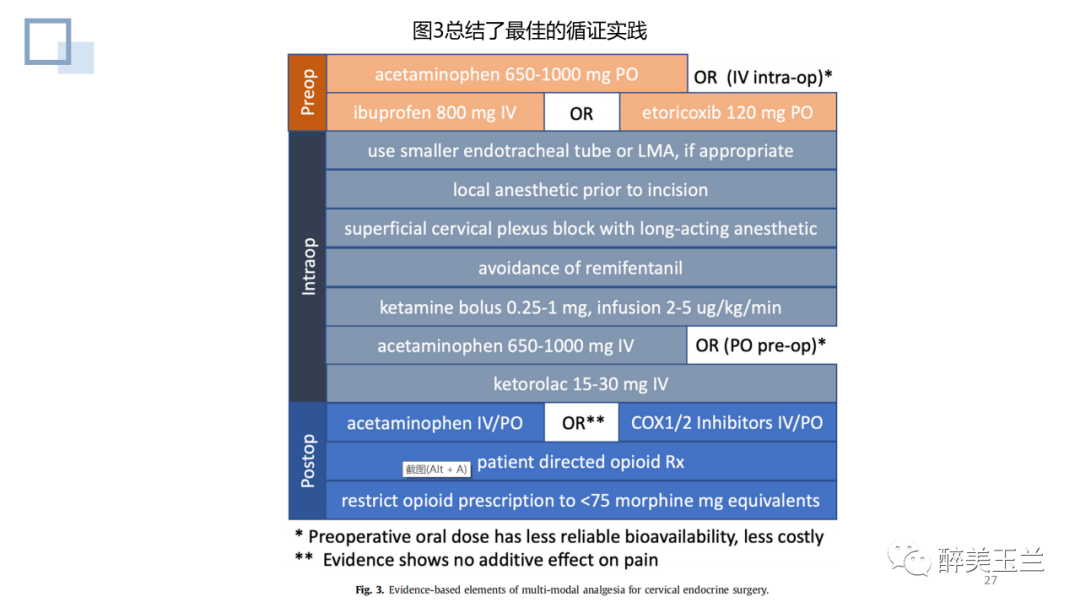
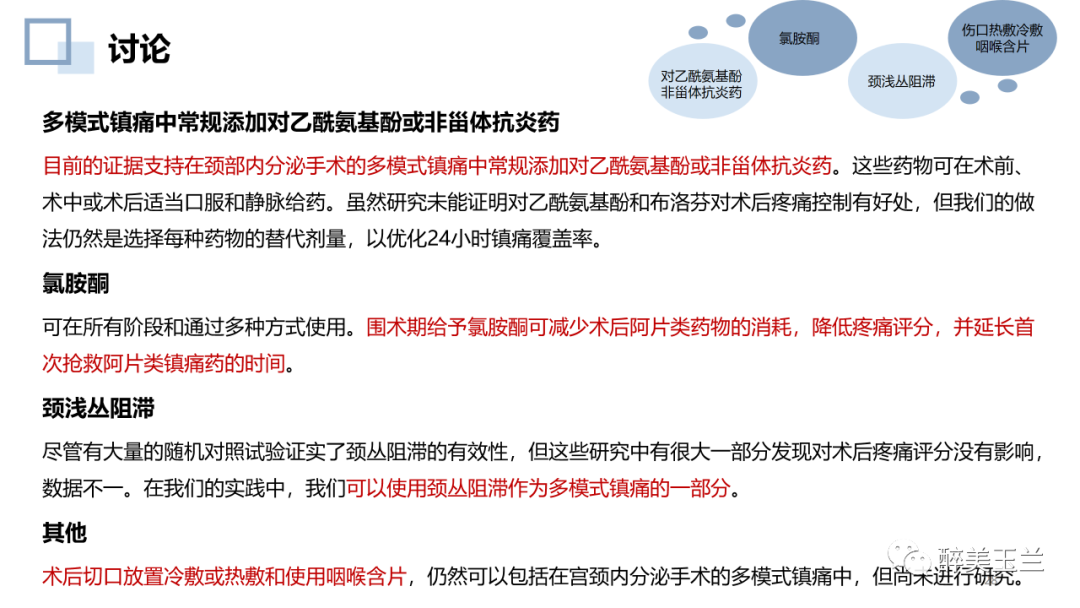
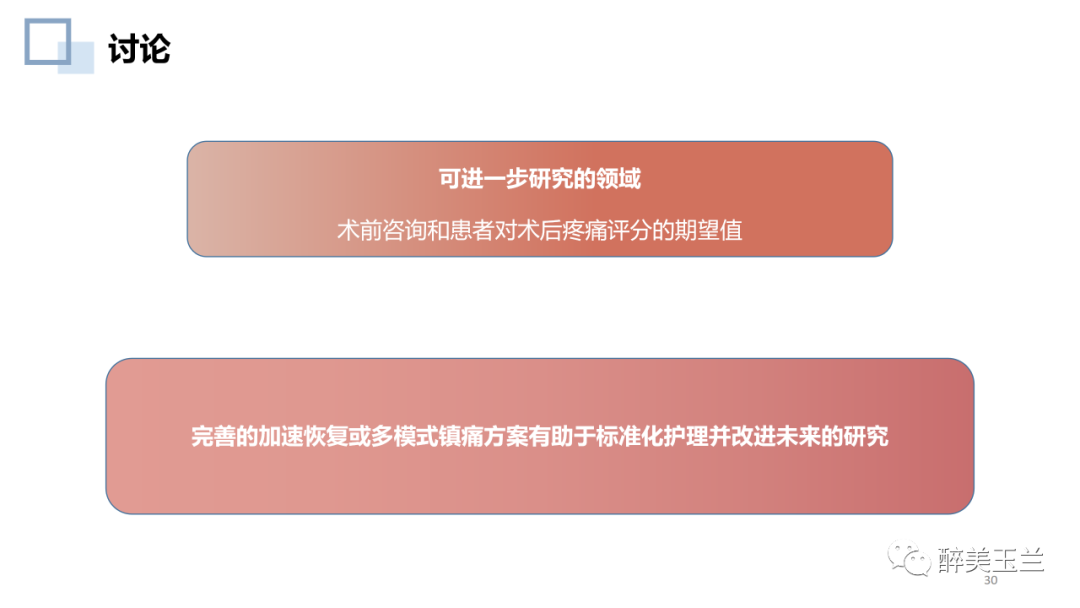
本文回顾总结了颈部手术多模式镇痛最佳的循证实践,结果显示:气管插管表面麻醉、颈部神经阻滞、避免术中使用瑞芬太尼、多模式镇痛中常规添加对乙酰氨基酚或非甾体抗炎药、围术期给予氯胺酮、术后切口放置冷敷或热敷和使用咽喉含片是对行颈部手术患者围术期镇痛管理的要素。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
31
#疼痛管理#
55
#系统综述#
44
学习了
48
#手术期#
48
学习了
46
#甲状旁腺#
37
#甲状旁腺手术#
0
#学习#
63