新版医保目录自3月1日起执行,原研SGLT2抑制剂(艾托格列净)价格再创新低!
2021-03-07 医药魔方 医药魔方
新版国家医保目录将从2021年3月1日起开始在全国范围内正式启用。此次医保谈判共涉及162种药品,其中有119种药品谈判成功进入目录,谈判成功率为73.46%,谈成药品平均降价50.64%。
新版国家医保目录将从2021年3月1日起开始在全国范围内正式启用。此次医保谈判共涉及162种药品,其中有119种药品谈判成功进入目录,谈判成功率为73.46%,谈成药品平均降价50.64%。
除了备受关注的新冠、肿瘤、罕见病及儿童疾病领域新药进入目录外,慢病领域如糖尿病也有多款新药被纳入目录。其中,默沙东新一代钠葡萄糖协同转运蛋白2(SGLT2)抑制剂艾托格列净(捷诺妥?)也在此次谈判中顺利进入医保目录。
据了解,国内市场现有四种SGLT2抑制剂,均已被纳入国家医保。艾托格列净作为最晚进入中国市场的原研SGLT2抑制剂,在上市同年即被纳入国家医保,价格为3.46元/片,是现阶段医保目录中价格最低的原研SGLT2抑制剂。 SGLT2抑制剂——口服降糖药的新星
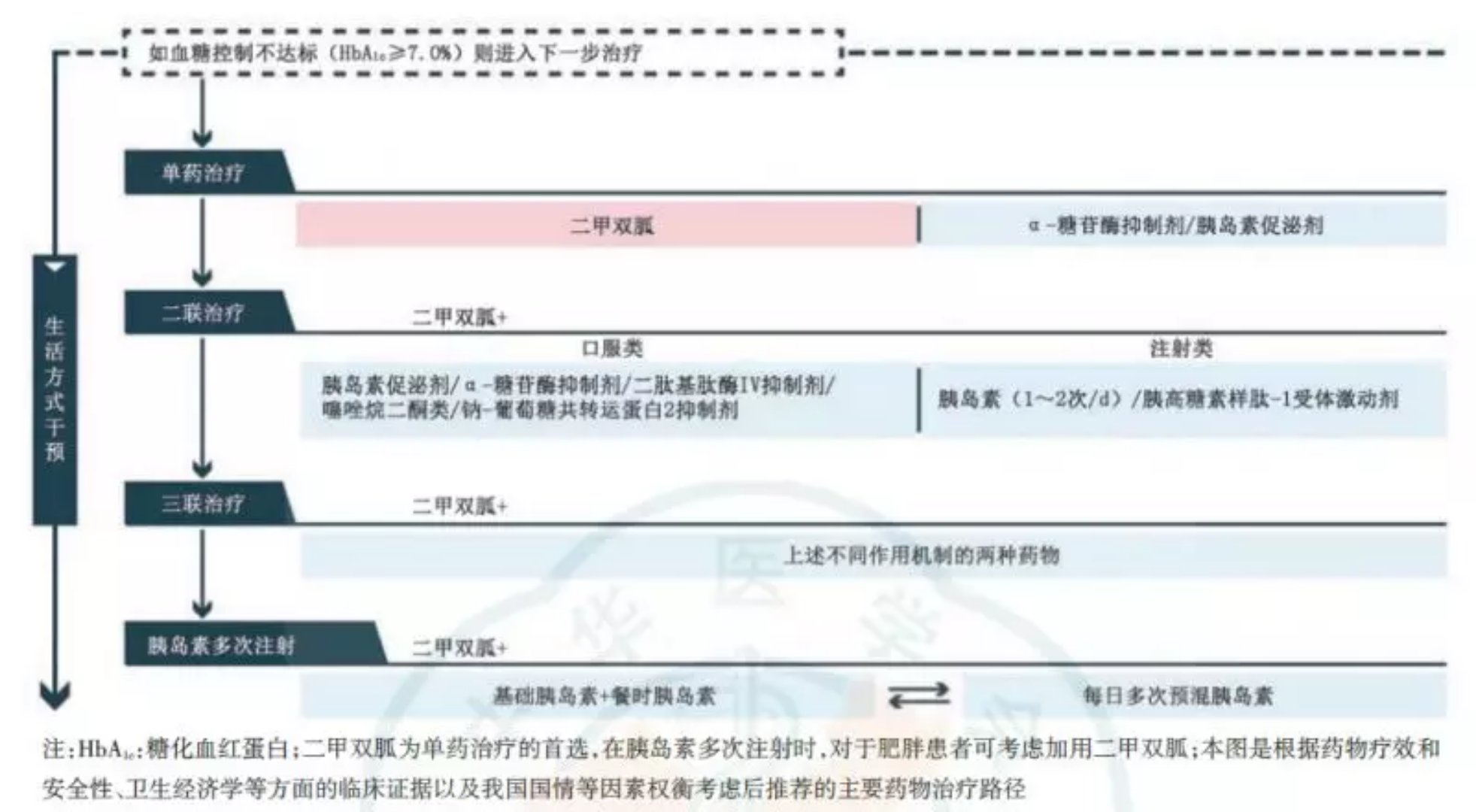
SGLT2抑制剂作为一种新型的口服降糖药,自上市之初起就获得了众多关注。它独特的作用机制,通过抑制肾小管葡萄糖重吸收来降低血糖水平,即通过肾脏排泄葡萄糖,因为不依赖胰岛素的多少和敏感性而受到患者和医师的推崇。同时,多项大型试验也证实了SGLT2抑制剂的心血管获益。它可显着降低2型糖尿病患者心血管疾病风险,改善2型糖尿病患者的心血管结局。基于SGLT2抑制剂的心血管和肾病获益,美国糖尿病学会发布的《糖尿病诊疗标准(2021年版)》建议,将SGLT2抑制剂作为2型糖尿病合并动脉粥样硬化性心血管疾病、心衰、慢性肾病患者的推荐药物之一。 以艾托格列净为例,最新研究VERTIS CV结果表明,与安慰剂相比,治疗组研究结果达到了主要心血管不良事件(MACE)的非劣效性主要终点。MACE包括心血管死亡、非致命性心肌梗死或非致命性卒中。这一研究结果表明,对于患有心血管疾病的2型糖尿病患者,使用艾托格列净可降低他们因心衰住院的风险。
艾托格列净中国注册临床研究的负责人、北京大学人民医院内分泌科主任纪立农教授指出:肾病和包括心衰在内的心血管疾病是糖尿病患者的常见并发症,也是导致糖尿病患者死亡的重要原因。因此对于糖尿病患者来说,选择具有肾脏和心血管疾病保护作用的降糖药进行长期治疗是改善糖尿病患者健康结局的重要措施。随着国家对慢病防治的日益重视,像SGLT2抑制剂这样的新药得以快速进入医保,惠及广大患者。以艾托格列净为例,这次医保谈判后价格仅为3.46元/片,极大提高了该药物的可及性和可负担性,为患者带来了有效、安全、可付担的高性价比治疗选择。 口服降糖药市场群英逐鹿
糖尿病领域一直是大型药企争相竞夺的赛场之一。目前,在中国SGLT2抑制剂赛道上已有四家跨国药企率先布局。从各企业在糖尿病领域的综合竞争力上来看,默沙东除了最新上市的SGLT2抑制剂外,还拥有口服降糖药市场份额稳居第一的西格列汀产品(捷诺维?和捷诺达?)。西格列汀在全球上市15年,其独特的作用机制可以帮助糖尿病患者“唤醒”胰岛功能,实现内源性降糖,从而达到长期控糖的目标。同时,西格列汀还具有服药便捷、安全性高等优势,适用人群十分广泛。此次上市即被纳入医保的艾托格列净具有明显的临床优势和极富竞争力的产品价格,也将默沙东糖尿病产品线延伸至更加细分的人群,势必将助力其继续扩大在糖尿病领域的综合竞争力和业务版图。中国糖尿病市场未来争格局如何?我们拭目以待。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制剂#
42
#SGLT#
24
#2抑制剂#
37
#创新#
18
#医保目录#
28
#SGLT2#
20