STROKE:蛛网膜下腔出血的治疗新方法!
2017-09-16 MedSci MedSci原创
延迟性脑梗死(DCI)是动脉瘤蛛网膜下腔出血后发病率和死亡率的主要原因。近期,一项发表在杂志Stroke上的研究报告了一种新型干预立体定向导管脑室间隔切除术(STX-VCS)和纤维蛋白溶解/解痉灌洗治疗用于预防DCI的方法。此项研究将20例患者的结果与60例相匹配的对照组人群进行了比较。在受试个体做出治疗决定的基础上,自2015年9月至2016年10月期间,在20例高风险动脉瘤蛛网膜下腔出血患者中
延迟性脑梗死(DCI)是动脉瘤蛛网膜下腔出血后发病率和死亡率的主要原因。近期,一项发表在杂志Stroke上的研究报告了一种新型干预立体定向导管脑室间隔切除术(STX-VCS)和纤维蛋白溶解/解痉灌洗治疗用于预防DCI的方法。
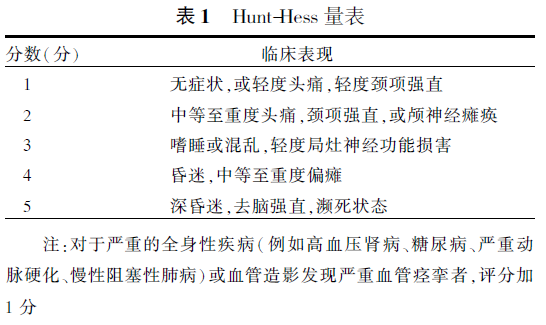
此项研究将20例患者的结果与60例相匹配的对照组人群进行了比较。在受试个体做出治疗决定的基础上,自2015年9月至2016年10月期间,在20例高风险动脉瘤蛛网膜下腔出血患者中进行了STX-VCS。三名按照年龄、性别、动脉瘤治疗方法和入院Hunt和Hess级别被分配到由STX-VCS处理的每个病例中。 DCI是此项研究主要的结果。康复出院的死亡率和mRS是次要结局参数。通过条件逻辑回归评估STX-VCS与DCI、死亡率和mRS之间的联系。
此项研究结果显示:立体定向手术没有手术并发症。 20例患者中有17例(85%)可以进行持续灌洗。一例出现不良事件但没有后遗症。在60例(42%)对照组中有25例发生了DCI,20例(15%)STX-VCS患者中有3例(优势比,0.15; 95%置信区间,0.04-0.64)。 60例(33%)对照组中的20例以及20例STX-VCS组中的1例(5%)患者分别出现死亡(优势比,0.08; 95%置信区间,0.01〜0.66)。20例STX-VCS(60%)患者中的12例(60%)有良好的治疗结局(mRS≤3) ,而60例对照组中有21例(35%)出现良好的治疗结局(优势比,0.26; 95%置信区间,0.8-0.86)。
此项研究结果表明:STX-VCS在严重动脉瘤蛛网膜下腔出血患者中是可行的和安全的。初步结果表明,该方法可以降低DCI和死亡率,并且可以通过该方法的治疗改善患者神经学的结果。
原始出处:
Roelz R, Coenen VA, et al. Stereotactic Catheter Ventriculocisternostomy for Clearance of Subarachnoid Hemorrhage: A Matched Cohort Study. Stroke. 2017 Sep 13. pii: STROKEAHA.117.018397. doi: 10.1161/STROKEAHA.117.018397.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新方法#
23
#治疗新方法#
31
#蛛网膜#
24
文章是好文章翻译差了点..
51
非常好的文章.学习了
59
学习一下知识
62
非常好的文章.学习了
60
很好的文章.谢谢分享
46