JAHA:心率变异性在肾小球高滤过与全因死亡率之间关联中的作用
2021-12-12 MedSci原创 MedSci原创
心率变异性降低与肾小球高滤过之间存在独立相关性。在既往没有心血管事件的个体中,自主神经功能障碍可能与肾小球高滤过不良结局的发病机制有关。
肾小球高滤过与健康个体的心血管事件增加相关,但发病机制尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是调查肾小球高滤过是否与受试者的死亡率相关,以及心率变异性降低是否与肾小球高滤过相关。
研究人员回顾性地分析了1615名既往没有心血管事件的参与者(平均年龄为66.1±17.3岁,61.9%为男性)。研究人员使用慢性肾脏病流行病学合作方程估计了肾小球滤过率。肾小球高滤过定义为肾小球滤过率在年龄和性别分层后的第95个百分位数以上,而正常滤过定义为第25至第75个百分位数。研究人员使用24小时动态心电图测量了心率变异性指标,包括时域、频域和样本熵。临床结据为2年时的全因死亡率。
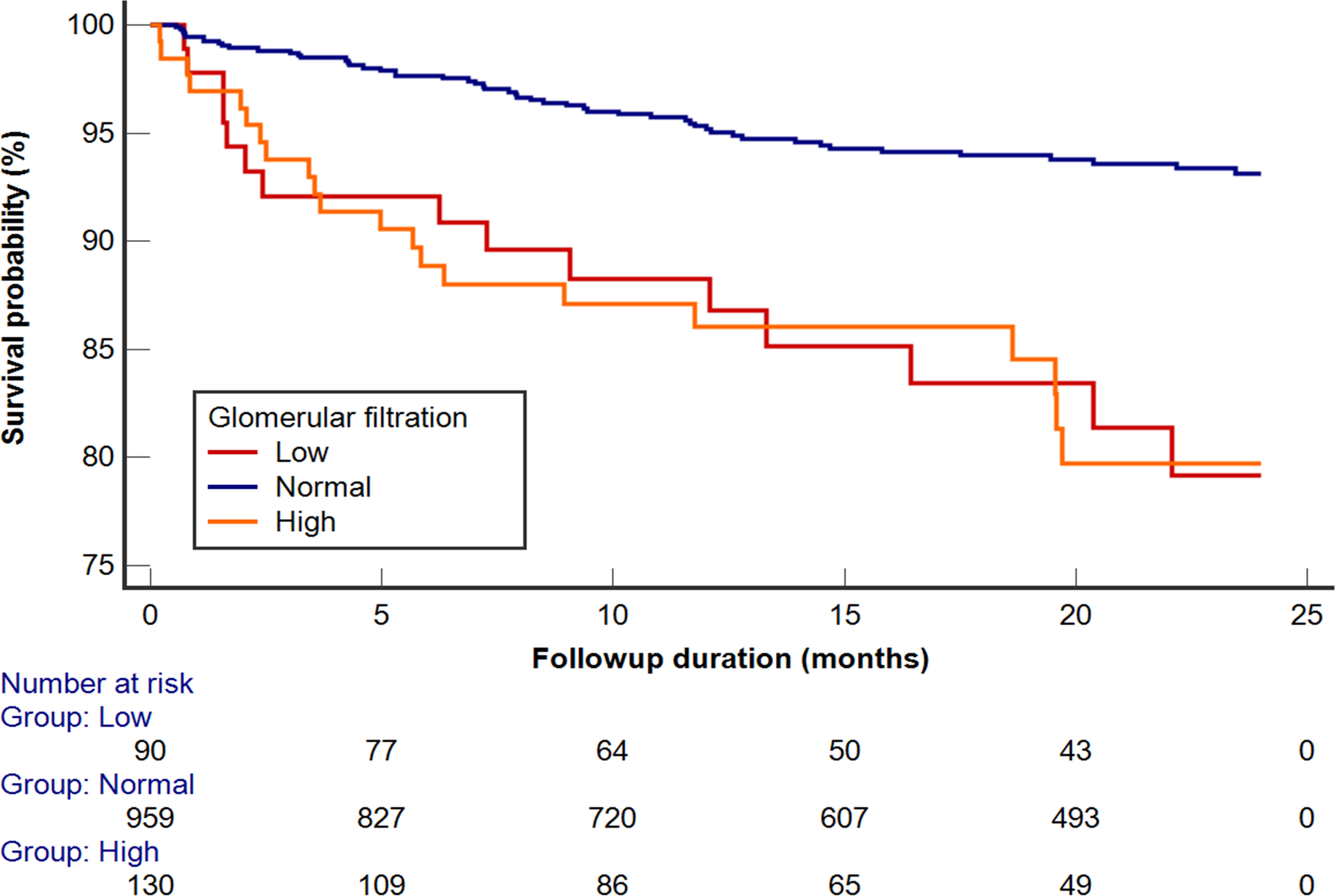
在平均16.5±8.2个月的随访期间,有117名参与者死亡(7.2%)。肾小球高滤过与参与者更高的死亡风险相关(风险比和95%CI为1.97[1.15–3.37])。在考虑年龄、性别、平均心率、发病率和药物后,降低的心率变异性指数,包括时域、频域和样本熵(比值比和95%CI为0.79[0.70-0.89])均与肾小球高滤过独立相关。在亚组分析中,与老年人相比,年轻参与者的心率变异性降低能更好地预测肾小球高滤过。介导分析揭示了心率变异性和肾小球高滤过之间的显著的介导作用,以及它们各自对生存具有不利效应。
由此可见,心率变异性降低与肾小球高滤过之间存在独立相关性。在既往没有心血管事件的个体中,自主神经功能障碍可能与肾小球高滤过不良结局的发病机制有关。
原始出处:
Hao‐Chih Chang,et al.Role of Heart Rate Variability in Association Between Glomerular Hyperfiltration and All‐Cause Mortality.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021585
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#全因死亡率#
50
#AHA#
26
#变异#
33
#心率变异性#
46