北京友谊医院完成世界首例肾衰患者胸骨下段小切口冠脉旁路移植术
2015-12-11 郑杨 崔永超 医学论坛网
日前,北京友谊医院心血管中心心脏外科成功完成世界首例肾功能衰竭患者的胸骨下段小切口冠状动脉旁路移植术。 年近60的周先生近一个月来胸闷、胸痛症状逐渐加重,辗转就诊于北京的各大医院。因患者慢性肾功能不全(尿毒症期)维持性血液透析,慢性肾小球肾炎,阵发性心房颤动,高血压3级(极高危组),且于半年前曾放入三个心脏支架后再次出现急性非ST段抬高型心肌梗死,心律失常。多家医院表示患者合并症多,手术风险

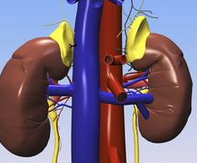
日前,北京友谊医院心血管中心心脏外科成功完成世界首例肾功能衰竭患者的胸骨下段小切口冠状动脉旁路移植术。
年近60的周先生近一个月来胸闷、胸痛症状逐渐加重,辗转就诊于北京的各大医院。因患者慢性肾功能不全(尿毒症期)维持性血液透析,慢性肾小球肾炎,阵发性心房颤动,高血压3级(极高危组),且于半年前曾放入三个心脏支架后再次出现急性非ST段抬高型心肌梗死,心律失常。多家医院表示患者合并症多,手术风险大,没有能力救治像他这样的危重患者。周先生经多方了解后得知北京友谊医院心外科对于心脏外科危重症,尤其是合并重要脏器功能不全的心脏病患者的手术治疗在业界享有盛誉,遂抱着一线希望来到首都医科大学附属北京友谊医院心外科张永主任的诊室就诊。
专家详细了解周先生的病情后,即刻将患者收入心血管中心心外科治疗。在完善各项相关检查后,进一步明确了患者的病情,心外科主任张永教授及团队经过缜密分析病情和研究,明确了手术指证,但手术难度极大。因手术复杂,患者已患尿毒症多年并进行血液透析治疗,围术期极有可能出现多脏器功能衰竭,危及生命。考虑到患者的生命安危与生存质量,在与患者及家属进行了全面细致的沟通后,心外科的专家们勇担风险,决定采取积极的手术治疗,并制定了缜密的手术方案,完善了各项术前准备。
由于患者病情危重,对循环平稳及水电解质平衡的要求极高,麻醉科安排了具有丰富危重症心脏外科麻醉经验的洪方晓教授亲自主持麻醉,严密观察常规心电监护、动脉有创血压、中心静脉压、漂浮导管检查、心输出量测定、BIS脑电双频指数等各项监护指标。麻醉过程非常平稳。在手术室心外手术组密切配合下,进行了胸骨下段小切口不停跳冠状动脉旁路移植术。
术中发现患者由于多年的尿毒症,水电解质代谢紊乱,组织存在异常钙化,解剖间隙已发生改变,组织僵硬脆弱,尤其是冠脉,稍有不慎就会发生致命性的大出血。张永主任在手术放大镜下,采用小针细线,极其流畅的完成了多个吻合口的吻合,一气呵成,术中共搭桥3支。整个手术过程仅仅耗时不足5个小时。患者多年的尿毒症导致凝血功能障碍,经过麻醉科洪方晓教授的精心调整,术中出血不足300毫升。经多方紧密配合,共同努力,患者术中循环稳定,术后病人安返重症医学监护室。
重症医学科安排了精兵强将进行围术期调整,迅速完成穿刺置管进行持续性血液滤过,保证了患者循环、呼吸功能的稳定及水电解质代谢的平衡。术后患者恢复顺利,在预期内拔除了气管插管并进行了机体功能康复锻炼,血管外科朱仁明医生在住院期间为患者完成了桡动脉造瘘术,为患者后期进行血液透析治疗打下来坚实的基础。目前患者复查心肺肾等重要脏器功能稳定,顺利出院。
出院时,周先生握着医护人员的手激动地说,“是你们这支优秀的团队给了我第二次生命,你们这些白衣天使就是我的亲人啊!”
该例手术的顺利完成充分体现了该院心脏外科,麻醉科、手术室及重症医学监护室等科室处理重症复杂患者的综合能力,保证了心脏外科在危重症的处理能力上处于国内领先地位,缩短了与国外顶级心脏中心的差距。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#旁路移植术#
36
#移植术#
28
#世界首例#
33
#北京友谊医院#
34
#友谊医院#
33
很值得学习
117
好文章,值得看。
108
…………
111
现在都在搞微创,高精尖。。。
117