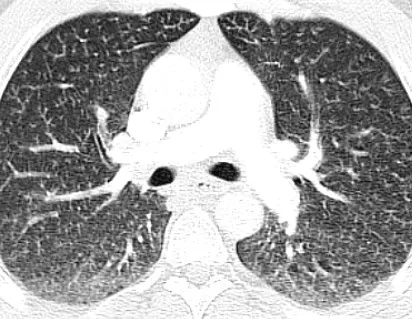
病例分享| 一例罕见的胃动静脉畸形
2019-03-28 多巴胺 医博士网
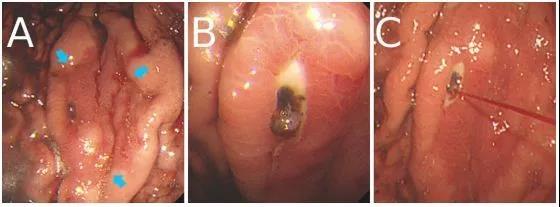
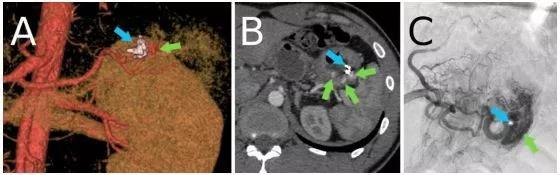
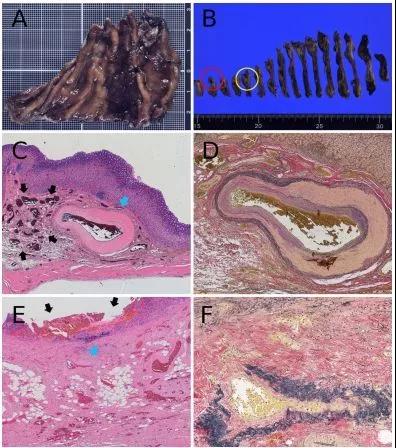
胃动静脉畸形(AVM)是上消化道出血的罕见原因,常引起上消化道出血并需要手术治疗。胃AVM的内镜检查结果尚未有明确指南,也很少有文献报道。本病案报道了一例罕见的胃AVM病例,通过胃十二指肠镜发现,经手术治愈。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#动静脉畸形#
29
#静脉#
25
#畸形#
32
#罕见#
21