Sci Transl Med:突破:新药在化疗前“软化”肿瘤,可使癌症存活率翻倍
2017-04-07 Heather_z727 medicalnewstoday
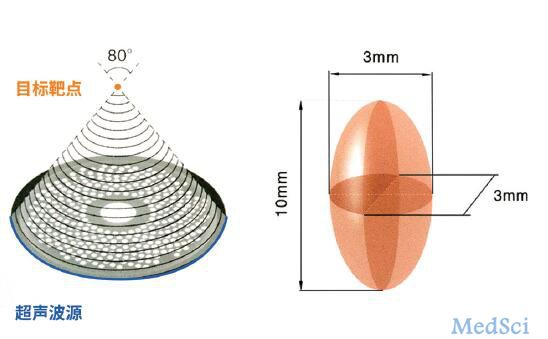
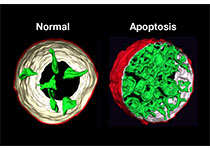
【法舒地尔:软化癌细胞周围组织,使化疗效果最大化】最新的一项研究表明,一种药物可以在化疗之前“软化肿瘤”,在胰腺癌小鼠实验中,这种药物减少了肿瘤扩散,使生存几率翻倍。来自澳大利亚研究小组的此次研究结果发表于《科学转化医学》杂志中。胰腺癌始于胰腺细胞内,胰腺包含两个主要类型的细胞:外分泌细胞负责消化酶,内分泌细胞控制激素,比如胰岛素和控制血糖的胰高血糖素。胰腺癌的致病因素目前尚不明确,但随着不断的研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#存活率#
0
#TRA#
30
#Transl#
36
#Med#
30
学习了谢谢分享
50