JAMA Pediatr:新生儿服用益生菌可降低功能性肠胃病风险
2014-01-15 koo 生物360
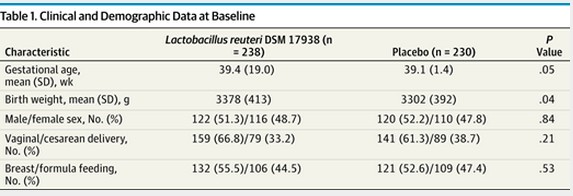
周一发布的一份研究结果显示,向新生儿肠道引入益生菌似乎可以降低他们发生肠绞痛的几率。这是显示益生菌有助缓解肠绞痛的最新研究结果。该研究被认为是首次检验新生儿服用益生菌能否预防功能性肠胃病发生的研究,功能性肠胃病包括肠绞痛、返流和便秘。 肠绞痛被认为与消化问题有关,有时被解释为婴儿的肠易激综合征,往往伴随新生儿的长时间哭闹。这种状况一直是新生儿父母焦虑的原因,在没有针对性治疗药物的情况下,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
37
#DIA#
35
#肠胃病#
50
#功能性#
31
#胃病#
38