Sci Rep:孕妇高果糖饮食可能对胎儿有不利影响
2016-05-07 MedSci MedSci原创
怀孕期间高果糖饮食可能会导致胎盘缺陷以及限制胎儿的生长,这无形中增加了婴儿以后的健康风险。不过,通过给予小鼠别嘌醇后发现,这似乎能够缓解孕妇的这种习惯带来的对胎儿不利影响。调查的结果提示高果糖摄入的产妇进行产前筛查是必要的。该研究结果发表在自然出版集团下属期刊《Scientific Reports》上。果糖是水果和蜂蜜中天然存在的一种糖类。糖果工业中已经将果糖玉米糖浆作为添加剂使用了几十年。果糖在

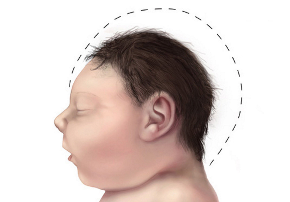
怀孕期间高果糖饮食可能会导致胎盘缺陷以及限制胎儿的生长,这无形中增加了婴儿以后的健康风险。
不过,通过给予小鼠别嘌醇后发现,这似乎能够缓解孕妇的这种习惯带来的对胎儿不利影响。调查的结果提示高果糖摄入的产妇进行产前筛查是必要的。
该研究结果发表在自然出版集团下属期刊Scientific Reports上。
果糖是水果和蜂蜜中天然存在的一种糖类。糖果工业中已经将果糖玉米糖浆作为添加剂使用了几十年。果糖在体内的代谢方式与葡萄糖不同,葡萄糖通常转换为能量,而果糖通常由肝细胞分解后转化为甘油三酯,同时驱动尿酸的合成增加。尿酸含量的大量增加将会引起代谢紊乱,诱导痛风、糖尿病等发生。通过动物实验,研究人员发现孕期小鼠进行高果糖饮食后体内尿酸和甘油三酯含量增加。
为了探索动物实验的结论是否在人类身上也会重现,研究人员对18例剖腹产妇女体内果糖水平和尿酸含量相关性进行了研究。这些妇女没有能够引起尿酸增加的代谢综合征。结果发现,这种相关性在人类中也出现了。
现有的证据支持孕妇体内多余的果糖可能会造成某种程度上的不利影响。研究者建议孕妇限制果糖量的摄入。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












深入学习,好文值得点赞!
66
学习了,很好的
177
学习了,很好的
106
文章不错
122
值得学习
82