JAHA:疾病特异性健康状况与外周动脉疾病患者长期生存之间的关系
2022-02-11 MedSci原创 MedSci原创
PAD特异性健康状况与新出现或症状恶化的PAD患者5年生存率独立相关,最近的评估是最具预测意义的。未来的工作需要更好地了解如何主动使用这些信息来优化PAD的治疗。
外周动脉疾病(PAD)仍然是一种未被充分认识和治疗的疾病,尽管它具有较高的心血管发病和死亡风险,1年事件发生率超过21%。随着疾病的进展,PAD患者可能会出现间歇性跛行和严重的肢体缺血,严重损害患者的功能和生活质量。

在有症状的患者中,想获得症状缓解和患者健康状况的改善往往是PAD患者寻求血管专科治疗的主要原因。虽然外周动脉疾病(PAD)与心血管疾病发病率增加有关,死亡率仍然很高且难以预测,但准确了解PAD患者诊断时一系列的特异性健康状况可能可以预测长期死亡风险。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员纳入了2011年至2015年期间在美国10个地区的PORTRAIT登记中心注册的新的或症状恶化的PAD患者。健康状况通过基线、3个月以及从基线到3个月随访的外周动脉问卷(PAQ)总结评分进行评估。研究人员使用3个月标志性和分层Cox回归模型构建了Kaplan-Meier,以评估PAQ与5年全因死亡率之间的关联。
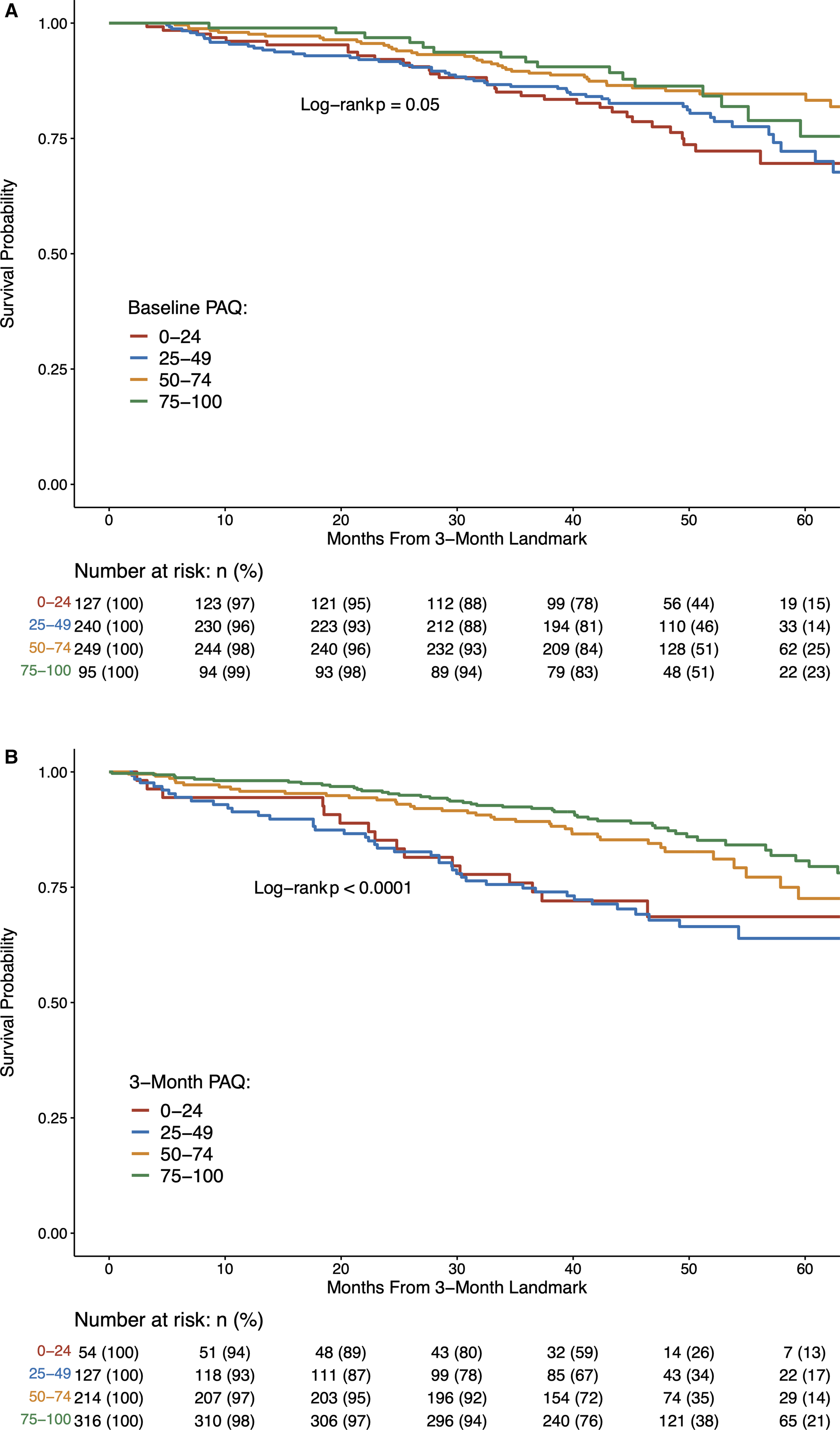
在711名患者中(平均年龄为68.8±9.6岁,40.9%为女性,72.7%为白人;基线和3个月的平均PAQ分别为47.5±22.0和65.9±25.0),141名(19.8%)患者在长达4.1年的中位随访期间死亡。在未经调整的模型中,基线(每增加10分对应的HR为0.90;95%CI为0.84-0.97;P=0.008)、3个月(HR[95%CI]为0.87[0.82-0.93];P<0.001)和PAQ的变化(HR[95%CI]为0.92[0.85-0.99];P=0.021)均与死亡率相关。在包括评分组合在内的完全调整模型中,3个月PAQ与死亡率之间的相关性强于基线(3个月HR[95%CI]为0.85[0.78-0.92];P<0.001;C统计量为0.77)或变化值(3个月HR[95%CI]为0.79[0.72-0.87];P<0.001)。
由此可见,PAD特异性健康状况与新出现或症状恶化的PAD患者5年生存率独立相关,最近的评估是最具预测意义的。未来的工作需要更好地了解如何主动使用这些信息来优化PAD的治疗。
原始出处:
Andy T. Tran.et al.Association of Disease‐Specific Health Status With Long‐Term Survival in Peripheral Artery Disease.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022232
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疾病患者#
42
#特异性#
32
#AHA#
41
#健康状况#
0
#外周动脉#
43
#长期生存#
32