Circ-Heart Fail:Tafamidis对甲状腺素运载蛋白淀粉样变心肌病患者长期生存的疗效
2021-12-29 MedSci原创 MedSci原创
最初在ATTR-ACT试验中接受Tafamidis治疗的患者的生存率明显高于最初接受安慰剂治疗的患者,这突出了早期诊断和治疗对于转甲状腺素蛋白淀粉样变心肌病的重要性。
Tafamidis(Fx1006A)是转甲状腺素蛋白动力稳定剂,能抑制淀粉样级连反应。在许多国家Tafamidis被批准用于治疗转甲状腺素蛋白淀粉样变心肌病。

近日,心血管领域权威杂志Circ-Heart Fail上发表了一篇研究文章,该研究报告了Tafamidis治疗转甲状腺素蛋白淀粉样变心肌病患者的长期疗效数据。
完成ATTR-ACT试验的转甲状腺素蛋白淀粉样变心肌病患者可以参加长期扩展分析(LTE),继续使用相同的Tafamidis剂量,或者如果之前接受过安慰剂治疗,则随机(2:1)接受80或20mg Tafamidis葡甲胺治疗。在协议修订后,LTE中的所有患者都过渡到61mg Tafamidis游离酸(生物等效于80mg Tafamidis葡甲胺)。在这项中期分析中,研究人员评估了在LTE中继续接受ATTR-ACT中80mg Tafamidis葡甲胺治疗患者的全因死亡率,并与在ATTR-ACT试验中接受安慰剂治疗的患者进行比较。
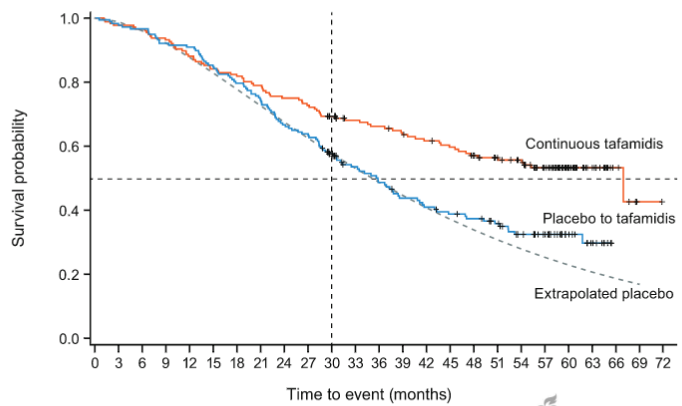
Tafamidis组(n=176)和安慰剂组(n=177)中位随访时间分别为58.5个月和57.1个月。连续Tafamidis治疗组有79例(44.9%)死亡,安慰剂转化为Tafamidis组有111例(62.7%)死亡(风险比为0.59[95%CI为0.44-0.79];P<0.001)。相对于安慰剂转化为Tafamidis组,连续Tafamidis治疗亚组的死亡率也降低:变异型转甲状腺素蛋白淀粉样变性(0.57[0.33-0.99];P=0.05)和野生型转甲状腺素蛋白淀粉样变性(0.61[0.43-0.87];P=0.0)以及基线纽约心功能分级I级和II级(0.56[0.38-0.82];P=0.003)和III级(0.65[0.41-1.01];P=0.06)。
由此可见,最初在ATTR-ACT试验中接受Tafamidis治疗的患者的生存率明显高于最初接受安慰剂治疗的患者,这突出了早期诊断和治疗对于转甲状腺素蛋白淀粉样变心肌病的重要性。
原始出处:
Perry Elliott,et al.Long-Term Survival With Tafamidis in Patients With Transthyretin Amyloid Cardiomyopathy.Circulation:heart failure.2021.https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.120.008193
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
31
#ART#
42
#淀粉样变#
33
#HEART#
26
#长期生存#
33
#肌病#
27