Pain:癌症患者中出现慢性疼痛的患病率和发病率
2017-03-10 MedSci MedSci原创
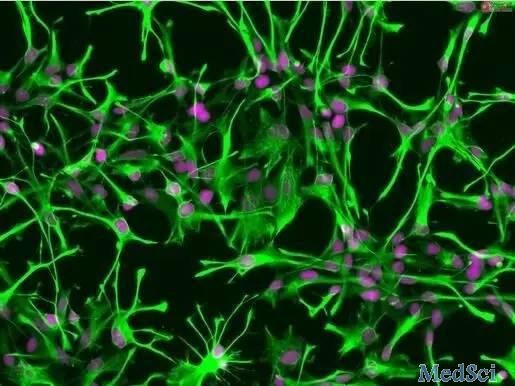
近期,发表在杂志Pain上的文章进行了一项前瞻性多中心研究,以估计在法国患有癌症的患者中具有或不具有神经病特征的慢性疼痛的患病率和发病率。此项研究招募了12个肿瘤学单位中癌症治疗进行两周内观察的所有连续门诊患者(n = 1885),共包括1805名患者。患者在访视1期间进行临床检查,并完成问卷以检测慢性疼痛(定义为每日疼痛,至少三个月)及其强度,位置和神经病特征(即DN4得分≥4)。疼痛对生活质量
近期,发表在杂志Pain上的文章进行了一项前瞻性多中心研究,以估计在法国患有癌症的患者中具有或不具有神经病特征的慢性疼痛的患病率和发病率。
此项研究招募了12个肿瘤学单位中癌症治疗进行两周内观察的所有连续门诊患者(n = 1885),共包括1805名患者。患者在访视1期间进行临床检查,并完成问卷以检测慢性疼痛(定义为每日疼痛,至少三个月)及其强度,位置和神经病特征(即DN4得分≥4)。疼痛对生活质量的影响用简明疼痛量表进行评估。访视1期间无疼痛的患者被纳入发病率研究,并进行随后3个月和6个月时的随访。
研究结果显示:慢性疼痛的总发病率为28.2%[95%CI:26.3-30.5],范围为22.5%至35.4% ,这取决于原发性肿瘤的位置。这些患者中有20.9%的患者存在神经病变特征,根据原发肿瘤的位置,患病率为2.9%至9.7%。具有神经性特征的患者的疼痛强度和干扰更高。
根据原发性肿瘤位置,6个月随访期间的慢性疼痛的发生率为13%至28%,并且在19.9%的慢性疼痛患者中发现神经病特征。
原始出处:
Bouhassira D, Luporsi E, Krakowski I. Prevalence and incidence of chronic pain with or without neuropathic characteristics in patients with cancer. Pain. 2017 Mar 4. doi: 10.1097/j.pain.0000000000000895.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#发病率#
45
继续学习中,谢谢
48
#患病率#
27
#慢性疼痛#
27
#癌症患者#
32