J Clin Oncol:新型双特异性抗体ABBV-383在复发/难治性多发性骨髓瘤中初显疗效
2022-08-31 MedSci原创 MedSci原创
ABBV-383 在 RRMM 患者中的耐受性良好,剂量≥ 40 mg时,客观缓解率可达到 68%。这种新疗法在既往接受过多线治疗的患者中具有良好的初步抗肿瘤活性,值得进一步临床评估。
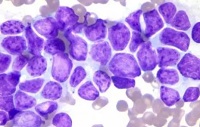
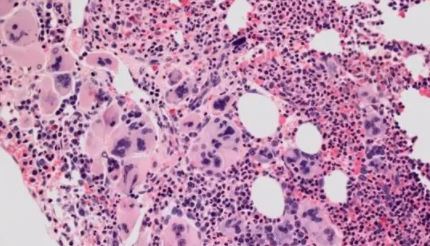
多发性骨髓瘤 (MM) 是全球第二大流行的血液系统恶性肿瘤。在过去的 20 年中,MM 的治疗选择有了显著改善,出现了许多新药,如蛋白酶体抑制剂、免疫调节药物、单克隆抗体。
ABBV-383 是一种 B 细胞成熟抗原 × CD3 T 细胞结合双特异性抗体,在正在进行的关于复发性/难治性多发性骨髓瘤(RRMM)的首次人体 I 期研究中显示出了可喜的结果。本文报告了该 I 期剂量递增/扩展研究的安全性和有效性结果。
该研究招募了既往至少接受过三线治疗(包括蛋白酶体抑制剂、免疫调节药物和抗 CD38 单克隆抗体)的 RRMM 患者,予以 ABBV-383 静脉滴注,每 3 周一次。并采用 3+3 设计进行剂量扩展。
截止 2022 年 1 月 8 日,共124位患者(剂量递增[0.025-120 mg],n=73;剂量扩展[60 mg],n=51)接受了 ABBV-383 治疗;中位年龄是 68 岁(范围 35-92岁)。最常见的血液学需紧急处理的不良事件(TEAE)有中性粒细胞减少症(37%)和贫血(29%)。最常见的非血液学 TEAE 有细胞因子释放综合征(57%)和疲劳(30%)。七位患者死于 TEAE,经判定均与研究治疗无关。
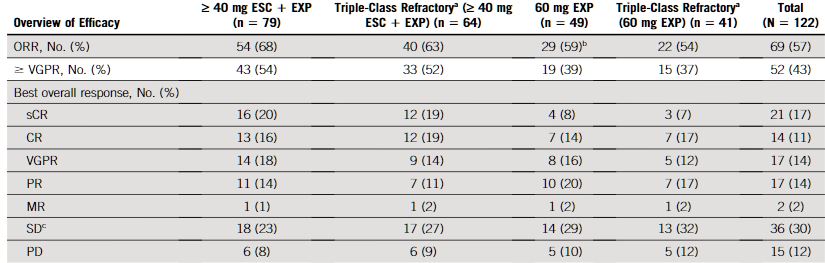
缓解率
在可评估疗效的患者(n=122)中,客观缓解率(ORR)是 57%,非常好的部分缓解或更好缓解(≥VGPR)率是43%。在 60 mg 剂量扩展队列(n=49),ORR 和 ≥VGPR 率分别是 59% 和 39%;在≥40 mg 剂量递增和剂量扩展队列(n=79)中,ORR 和 ≥VGPR 率分别是 68% 和 54%。
无进展生存率
综上,ABBV-383 在 RRMM 患者中的耐受性良好,剂量≥ 40 mg时,客观缓解率可达到 68%。这种新疗法在既往接受过多线治疗的患者中具有良好的初步抗肿瘤活性,值得进一步临床评估。
原始出处:
D'Souza Anita,Shah Nina,Rodriguez Cesar et al. A Phase I First-in-Human Study of ABBV-383, a B-Cell Maturation Antigen × CD3 Bispecific T-Cell Redirecting Antibody, in Patients With Relapsed/Refractory Multiple Myeloma.[J] .J Clin Oncol, 2022, undefined: JCO2201504.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Oncol#
54
#特异性#
77
#多发性#
64
#特异性抗体#
47
#难治性#
62