Open Heart:戒烟可降低CVD风险,甚至达到从不吸烟者水平
2016-10-25 MedSci MedSci原创
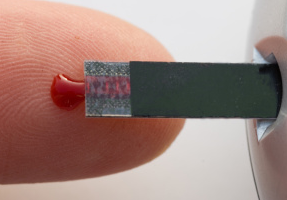
研究人员报告说,在芬兰的工作年龄人口中,过去或现在吸烟,对个体心血管(CVD)危险因素有临床上的较小的显著性影响。研究人员在Open Heart中写道,“在工作年龄戒烟可以减少CVD风险,甚至可以降低到与从不吸烟者相当水平。”参与者为3548名31-46岁人群。使用个体心血管疾病的危险因素、Framingham风险评分和冠心病风险评估系统(SCORE)计算在下一个十年中,患者的绝对CVD事件风险。
研究人员报告说,在芬兰的工作年龄人口中,过去或现在吸烟,对个体心血管(CVD)危险因素有临床上的较小的显著性影响。
研究人员在Open Heart中写道,“在工作年龄戒烟可以减少CVD风险,甚至可以降低到与从不吸烟者相当水平。”
参与者为3548名31-46岁人群。使用个体心血管疾病的危险因素、Framingham风险评分和冠心病风险评估系统(SCORE)计算在下一个十年中,患者的绝对CVD事件风险。
研究人员发现,从不吸烟者、最近戒烟者和以前吸烟者之间的心血管风险无显著差异。
在男性中,平均Framingham风险评分在46岁时,不吸烟者为7.5%,戒烟者为7.4%,以前吸烟者为8.1%,当前吸烟者为14.7%。
在女性中,平均Framingham风险评分在46岁时,不吸烟者为3.3%,戒烟者为3%,以前吸烟者为3.2%,当前吸烟者为5.9%。
研究人员还报告,对男性和女性使用SCORE,发现吸烟和致命性心血管事件风险增加之间的关联。
当研究人员分析随着时间的推移吸烟行为的变化,他们发现,30岁前戒烟的超过80%的个体,在46岁时,仍不吸烟。
总体而言,吸烟者与不吸烟者相比,体重指数和腰围增加。在男性中,目前吸烟者与从不吸烟者相比,有较高的总胆固醇和甘油三酯;在女性中,目前吸烟者与从不吸烟者相比,有较差的血脂水平、更高的低密度脂蛋白和甘油三酯,和较低的高密度脂蛋白。
女性目前吸烟者或最近戒烟者更容易使用降血脂药物。在男性中,先前吸烟者有最高的收缩压和舒张压,更容易使用抗高血压的药物。在女性中,不吸烟者有最高的收缩期血压水平。在男性中,先前和目前吸烟者的2型糖尿病的发病率是相似的;在女性中,也没有观察到差异。
研究人员写道:“与不吸烟者相比,吸烟者和戒烟者的吸烟相关危险因素很多;然而,这些主要的差异是很小的,不可能有重大的临床意义。”
原始出处:
Keto J, et al. Cardiovascular disease risk factors in relation to smoking behaviour and history: a population-based cohort study.Open Heart. 2016;doi:10.1136/openhrt-2015-000358.
Quitting smoking at working age may reduce CVD risk to same level as never-smokers.Healio.October 24, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
36
#CVD风险#
51
#ART#
24
#HEART#
40
#吸烟者#
33