Kidney Int:治疗狼疮性肾炎的新曙光!
2017-11-08 MedSci MedSci原创
最近的一项临床研究表明,由霉酚酸酯、他克莫司和类固醇组成的联合治疗显示,其较用静脉环磷酰胺和类固醇组成的常规疗法更能有效地使重度狼疮性肾炎患者达到完全缓解。近期,一项发表在杂志Kidney Int上的研究探索了此种联合治疗方案发挥增加疗效的分子和细胞机制,研究者们采用狼疮肾炎小鼠模型,MRL/lpr小鼠,并使用泼尼松、吗替麦考酚酯或他克莫司单药治疗或联合治疗。与此前的临床发现一致,与狼疮肾炎小鼠中
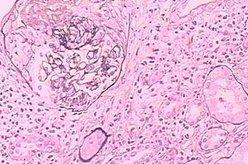
最近的一项临床研究表明,由霉酚酸酯、他克莫司和类固醇组成的联合治疗显示,其较用静脉环磷酰胺和类固醇组成的常规疗法更能有效地使重度狼疮性肾炎患者达到完全缓解。近期,一项发表在杂志Kidney Int上的研究探索了此种联合治疗方案发挥增加疗效的分子和细胞机制,研究者们采用狼疮肾炎小鼠模型,MRL/lpr小鼠,并使用泼尼松、吗替麦考酚酯或他克莫司单药治疗或联合治疗。与此前的临床发现一致,与狼疮肾炎小鼠中的单一疗法相比,联合疗法显着改善肾脏结果。小鼠肾脏组织的转录组分析揭示了其独特的分子途径,其在联合治疗法与单一疗法中有着差异调节。联合治疗方法不仅提供了附加的免疫抑制作用,而且诱导了基因表达和分子途径以赋予强化的肾脏保护作用。具体而言,联合治疗方法抑制了狼疮肾炎小鼠肾脏中TLR7的表达;他克莫司和霉酚酸酯的组合通过RhoA和Rac1活化的相互调节更好的稳定了足细胞肌动蛋白细胞骨架。此外,联合治疗还强烈抑制IL-6/Stat3途径。上述这些发现在霉酚酸酯、他克莫司或联合治疗前后狼疮肾炎患者的肾活检标本中进一步得到了验证。此项研究进一步提供了早期的临床发现,并进一步提供了增加狼疮性肾炎疗效的分子基
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#曙光#
41
#狼疮#
32
#肾炎#
27
#kidney#
35
学习了.涨知识
59
学习了.谢谢
59