European Radiology:基于机器学习的CT-FFR对TAVR术严重主动脉狭窄患者决策的影响
2022-08-24 shaosai MedSci原创
现阶段,临床上推荐使用冠状动脉计算机断层扫描(CCTA)进行冠状动脉的解剖学评估以确定假体的大小,并指导入口部位和方法的选择,同时排除CAD。
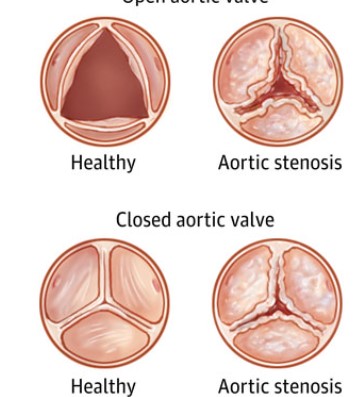
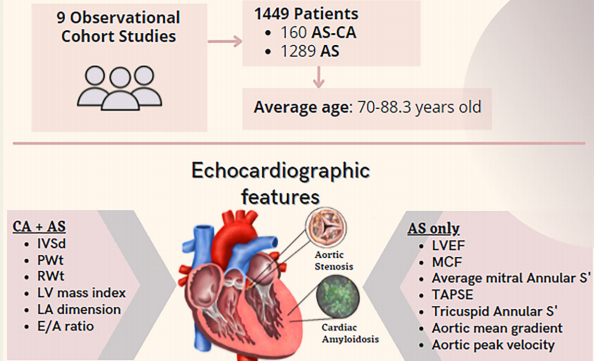
在合并主动脉瓣狭窄(AS)的患者中,冠状动脉疾病(CAD)的发生率在40-75%之间。因此,经导管主动脉瓣置换术(TAVR)前的诊断工作通常包括有创冠状动脉造影(ICA)以排除明显的CAD。然而在主动脉瓣狭窄患者中,有创分流量储备或瞬时无波比对决策的指导作用并没有得到明确解决。
现阶段,临床上推荐使用冠状动脉计算机断层扫描(CCTA)进行冠状动脉的解剖学评估以确定假体的大小,并指导入口部位和方法的选择,同时排除CAD。然而,仅仅通过使用CAD报告和数据系统(CAD-RADS)分类进行解剖学评估,在识别重要病变方面有其局限性,在存在严重钙化的斑块时尤为明显。
为了评估冠状动脉病变的功能情况,可以在ICA期间进行有创分流储备(FFR)评估,但需要额外的碘化对比剂、介入时间和辐射暴露。CCTA衍生的FFR(CT-FFR)是一种非侵入性的替代方法,在识别可从血管重建中获益的CAD患者方面具有很高的诊断准确性。
近日,发表在European Radiology杂志的一项研究评估了CT-FFR与CAD-RADS分类的可行性和诊断性能,以检测严重的AS患者接受TAVR时的重要CAD和决策,为临床治疗方案的制定及评估提供了参考。

本研究对接受术前TAVR-CT检查后进行ICA定量冠状动脉造影的连续严重AS患者(n = 95,78.6 ± 8.8岁,53%为女性)进行了回顾性分析。CCTA数据集使用CAD报告和数据系统(CAD-RADS)分类进行评估。使用现场机器学习算法计算CT-FFR测量值。根据TAVR前的CCTA,开发了一个联合算法用于决策以确定是否需要ICA。所有CAD-RADS≥4的患者都被转诊进行ICA,CAD-RADS 2和3的患者利用CT-FFR进行评估,如果CT-FFR≤0.80则进行ICA;CAD-RADS<2或CAD-RADS 2-3且CT-FFR正常的患者无需ICA。
12名患者(13%)在ICA上有明显的CAD(≥70%的狭窄),并接受了PCI治疗。28名患者(30%)显示CT-FFR≤0.80,其中24名(86%)报告了在ICA时最大狭窄度≥50%。使用所提出的算法,可以识别出重要的CAD,其敏感性、特异性、阳性和阴性预测值分别为100%、78%、40%和100%,相应减少了65次(68%)必要的ICA次检查。
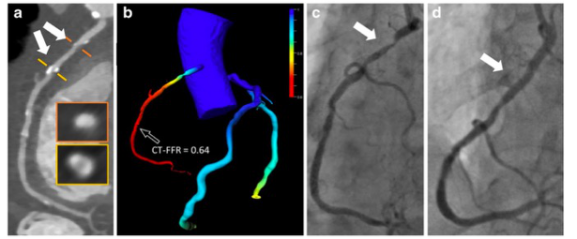
图 CCTA和ICA的冠状动脉狭窄以及使用机器学习的相应CT-FFR(CT-FFRML)示例。a 沿血管中心线自动生成的弧形多平面重建图显示右冠状动脉狭窄超过50%(基于直径的53%狭窄,基于面积的60%狭窄,CAD-RADS 3)。b 使用机器学习的冠状动脉树的彩色编码图显示CT-FFR值为0.64
本研究表明,在接受TAVR治疗的严重AS患者中,CT-FFR与CAD-RADS相结合可以可靠地识别术前CCTA上有功能意义的CAD,可大大减少术前ICA的数量,为规范TAVR的术前治疗流程、减少患者检查风险提供了支持。
原文出处:
Verena Brandt,U Joseph Schoepf,Gilberto J Aquino,et al.Impact of machine-learning-based coronary computed tomography angiography-derived fractional flow reserve on decision-making in patients with severe aortic stenosis undergoing transcatheter aortic valve replacement.DOI:10.1007/s00330-022-08758-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
58
#AVR#
36
#主动脉狭窄#
39
#主动脉#
51
#动脉狭窄#
38
#决策#
46
#机器#
43