67药品被重点监控,喜炎平、血栓通、小牛血……
2017-12-02 禹鑫 赛柏蓝
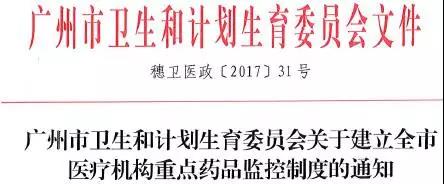
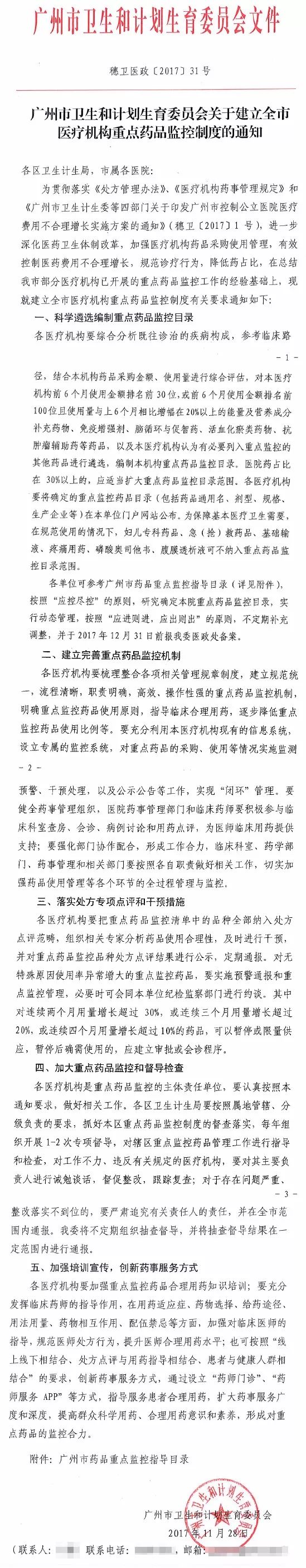
12月1日,一份广州卫计委《关于建立全市医疗机构重点药品监控制度的通知》,在业界传播。通知显示,其发布日期为11月28日。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
64
#喜炎平#
38
#血栓通#
42
#重点监控#
44
谢谢分享.学习了
50
好好好学习学习学习
67
这些药品是谁审批.让进入临床的
70
^_^^_^^_^
58
加強监管力度.保证用药安全
23
学习了新知识
31