JAMA Netw Open:胰高升糖素样肽-1受体激动剂与二肽基肽酶-4抑制剂的使用与2型糖尿病和晚期慢性肾脏疾病患者死亡率的关系
2022-03-21 从医路漫漫 MedSci原创
慢性肾脏病(CKD)和终末期肾病(ESKD)是造成健康负担的因素,并与增加的死亡率和心血管事件相关。
背景:慢性肾脏病(CKD)和终末期肾病(ESKD)是造成健康负担的因素,并与增加的死亡率和心血管事件相关。2型糖尿病是CKD的最常见原因,糖尿病和终末期肾病都与全因死亡率增加以及感染和心血管事件的增加有关。糖尿病合并CKD或ESKD患者的高死亡率主要归因于心血管或感染相关事件。胰高血糖素样肽-1(GLP-1)受体激动剂和钠-葡萄糖协同转运体-2(SGLT-2)抑制剂都与更好的血糖控制、更大的体重减轻、更低的死亡率和更低的死亡率有关。根据美国糖尿病协会的指南, GLP-1受体激动剂推荐用于估计肾小球滤过率低于60毫升/分钟/1.73平方米并有心血管疾病风险的糖尿病和CKD患者。根据肾脏疾病:改善2020年慢性肾脏疾病糖尿病治疗的临床实践指南,建议对无法使用二甲双胍或SGLT-2抑制剂的患者使用GLP-1受体激动剂治疗。与SGLT-2抑制剂不同,GLP-1受体激动剂可用于晚期CKD或ESKD患者。最近的一项网络荟萃分析7表明,在普通糖尿病人群中使用GLP-1受体激动剂和使用二肽基肽酶-4(DPP-4)抑制剂后,可能会有不同的临床结果。在该研究中,与使用DPP-4抑制剂相比,使用GLP-1受体激动剂与提高存活率有关。
然而,随机临床试验通常排除或纳入少量晚期CKD或ESKD患者。与此同时,DPP-4抑制剂通常被开给晚期CKD或ESKD患者,因为它们的安全性和血糖控制的有效性15尽管对肾脏和心血管结果有中性影响。然而,对于晚期CKD或ESKD患者,GLP-1受体激动剂治疗与提高生存之间的联系的讨论较少。此外,据我们所知,还没有真正的研究比较GLP-1受体激动剂和DPP-4抑制剂治疗晚期CKD或ESKD患者的疗效。在这项研究中,我们旨在评估在2型糖尿病和5期CKD或ESKD患者中使用GLP-1受体激动剂是否与使用DPP-4抑制剂相比具有更好的预后相关。
目的:评估在糖尿病和晚期CKD或ESKD人群中使用GLP-1受体激动剂是否与使用DPP-4抑制剂相比具有更好的预后相关。
方法:这项回溯性队列研究使用了从台湾国家健康保险研究数据库获得的关于2型糖尿病和CKD或ESKD的5期患者的数据。这项研究是在2012年1月1日至2018年12月31日之间进行的。对2020年6月至2021年7月的数据进行了分析。GLP-1受体激动剂与DPP-4抑制剂治疗暴露的比较。
主要结果和指标:比较了接受GLP-1受体激动剂治疗的患者和接受DPP-4抑制剂治疗的患者的全因死亡率、败血症和感染相关死亡率以及与主要不良心脑血管事件相关的死亡率。采用倾向性计分加权来缓解组间协变量之间的不平衡。
结果:27279例患者中,DPP-4抑制剂组265 578例(男性14443例,占54.34%;平均年龄65[13]岁);GLP-1受体激动剂组701例(男性346例,占49.36%;平均年龄59[13]岁)。加权后,GLP-1受体激动剂的使用与较低的全因死亡率(风险比[HR],0.79;95%CI,0.63-0.98)和较低的败血症和感染相关死亡率(HR,0.61;95%CI,0.40-0.91)相关。亚组分析显示,在脑血管疾病患者中,使用GLP-1受体激动剂与使用DDP-4抑制剂相关的死亡风险(HR,0.33;95%CI,0.12-0.86)低于非脑血管疾病患者(HR,0.89;95%CI,0.71-1.12)(交互作用P=0.04)。
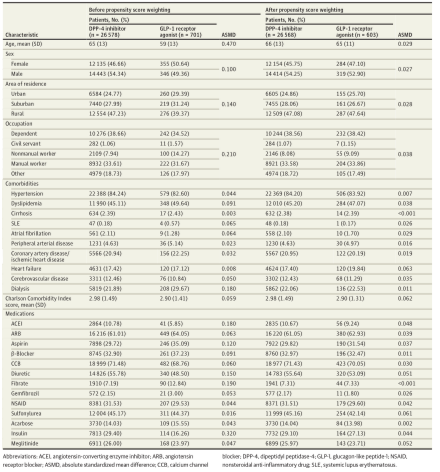
表1.糖尿病和5期慢性肾脏病或终末期肾病患者的基线特征
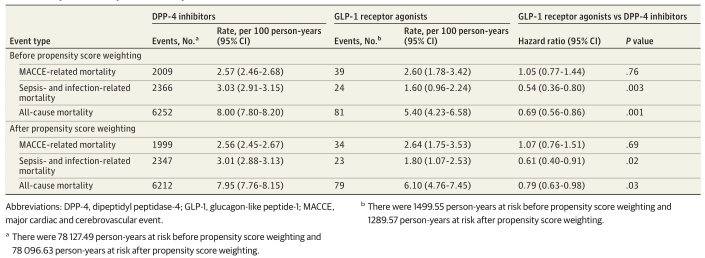
表2.对主要和次要结果的分析
结论:在2型糖尿病、晚期CKD和ESKD患者中,使用GLP-1受体激动剂的相关治疗比使用DPP-4抑制剂的患者全因死亡率更低。还需要更多精心设计的前瞻性研究来证实GLP-1受体激动剂治疗晚期CKD或ESKD患者的潜在益处。
原文出处: Chen JJ, Wu CY, Jenq CC, et al.Association of Glucagon-Like Peptide-1 Receptor Agonist vs Dipeptidyl Peptidase-4 Inhibitor Use With Mortality Among Patients With Type 2 Diabetes and Advanced Chronic Kidney Disease.JAMA Netw Open 2022 Mar 01;5(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者死亡#
36
#NET#
54
#抑制剂#
47
#疾病患者#
36
#二肽基肽酶-4抑制剂#
47
#PE#
26
#慢性肾脏#
37
#激动剂#
46