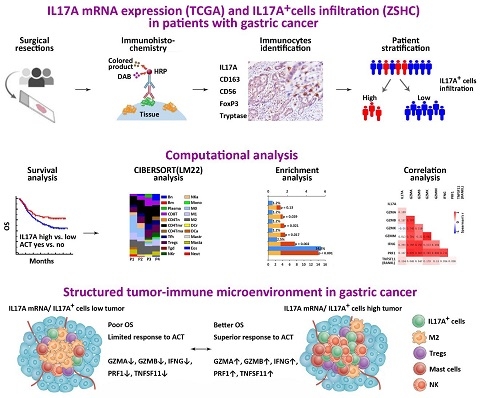
Ann Oncol:肿瘤浸润IL17阳性细胞 激活胃癌抗肿瘤免疫微环境和促进辅助化疗反应性
2018-12-08 佚名 复旦大学基础医学院
近期,复旦大学基础医学院徐洁杰课题组发现,在胃癌患者肿瘤组织中,肿瘤浸润IL17阳性细胞能够激活肿瘤微环境抗肿瘤免疫反应,促进胃癌患者术后辅助化疗反应性,该研究结果为胃癌患者的化疗选择和免疫治疗提供了新思路。11月15日,相关研究成果以“Intratumoral IL17-producing cells correlate with anti-tumor immune contexture and
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#反应性#
46
#Oncol#
31
#化疗反应#
50
#肿瘤免疫微环境#
53
学习了谢谢
61