西安交大二附院临床研究在美国引广泛关注
2017-06-20 雷恺 央广网
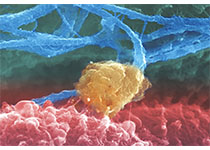
记者近日从西安交通大学第二附属医院获悉,西安交大二附院等联合开展的CAR-T治疗多发性骨髓瘤研究在美国临床肿瘤学会年会上引起广泛关注。这项研究的作者、西安交通大学第二附属医院的赵万红教授在一年一度的国际肿瘤学界盛会——美国临床肿瘤学会(ASCO)年会上介绍这项取得显着疗效的新型免疫治疗研究说,CAR-T是一种患者定制式治疗,即收集患者自身的T细胞,在体外进行基因重组,再回输到患者体内。基因重组的过
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#西安交大#
32
学习了,谢谢分享!
74
目前看到在淋巴瘤中疗效还可以
68
这样的研究很值得继续
101
学习,谢谢分享
59
多做些实在的研究
58
学习了。。。。。
21