J Clin Oncol:布伦妥昔单抗联合AVD方案治疗新确诊的有不良预后风险的早期霍奇金淋巴瘤
2021-04-29 MedSci原创 MedSci原创
4个疗程的BV和AVD联合方案在ES、有不良预后风险的霍奇金淋巴瘤患者中的耐受性良好,而且具有较高的治疗活性
长期以来,联合治疗方案被作为早期(ES)、有不良预后风险的肿块型霍奇金淋巴瘤(HL)的标准治疗方案,即化疗+放疗。但是,巩固放疗可能存在长期毒性,特别是对于纵膈,容易继发心肺疾病或恶性肿瘤。
为了提高新确诊的早期、有不良预后因素的霍奇金淋巴瘤的可治愈性并限制其长期不良反应,Kumar等人开展了一项包含了4个序贯队列的多中心研究。
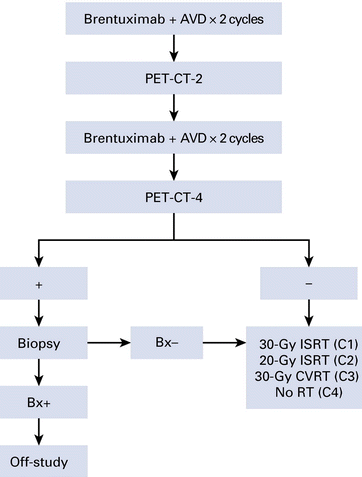
在该研究中,早期且具有不良预后风险的霍奇金淋巴瘤患者接受了4个疗程的布伦妥昔单抗(BV,也译本妥昔单抗)和阿霉素、长春碱和达卡巴嗪(AVD)治疗。如果PET-CT扫描阴性,则队列1的患者接受30 Gy剂量的定点放疗,队列2的患者接受20 Gy剂量的定点放疗,队列3的患者接受30 Gy剂量的综合区域放疗,队列4的患者不再接受放疗。主要终点是在队列1中评估安全性,在队列2-4中评估完全缓解率。
研究流程
共招募了117位患者,其中116位完成了化疗,中位年龄为32岁,50%的男性,98%的为II期,86%的为Memorial Sloan Kettering定义的肿块型(最大直径>7 cm),27%的为传统肿块型(>10 cm),52%的红细胞沉降率升高,21%的有结外浸润,56%的有>2个淋巴结浸润。
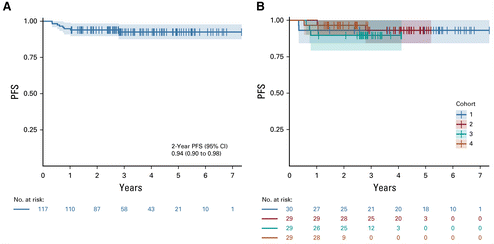
PFS和OS
队列1-4的完全缓解率分别为93%、100%、93%和97%。中位随访3.8年(5.9、4.5、2.5和2.2年),2年总无进展存活率和总存活率分别为94%和99%。队列1-4的2年无进展存活率分别为93%、97%、90%和97%。
不良反应包括中性粒细胞减少(44%)、发热性中性粒细胞减少(8%)和周围神经病变(54%),大部分不良反应是可逆的。
总之,4个疗程的BV和AVD联合方案在ES、有不良预后风险的霍奇金淋巴瘤患者中的耐受性良好,而且具有较高的治疗活性。BV联合AVD的疗效支持适当减少PET-CT扫描阴性患者的放射剂量。
原始出处:
Anita Kumar, et al. Brentuximab Vedotin Combined With Chemotherapy in Patients With Newly Diagnosed Early-Stage, Unfavorable-Risk Hodgkin Lymphoma. J Clin Oncol. April 28, 2021. https://ascopubs.org/doi/full/10.1200/JCO.21.00108
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
46
#不良预后#
35
#AVD#
46
认真学习了
65
精彩评论,需要您登录查看
79
谢谢梅斯分享这么多精彩信息
54
谢谢
65
好文章!
65